How ThoroughCare Helps Health Systems Monitor Care Transitions
Health systems are looking for ways to improve care outcomes and patient experiences while building cash flow and enhancing pay-for-performance.
Transitional Care Management and Remote Patient Monitoring offer concrete, evidence-based strategies to achieve these goals.
Through streamlined and standardized cloud-based software, health systems can pilot, launch, and scale effective care management programs by leveraging the care pathway between inpatient, ambulatory, and specialist clinics, as shown in Figure 1.

Figure 1: Health System model of care utilizing RPM and TCM.
Tailor Transitional Care Management program to health system goals
The health system’s structure and specific clinical, financial, and operational objectives drive which points of care should be included. Within the health system, a hospital could begin the Transitional Care Management workflow through its discharge process. Then, through direct or EHR interoperability with ThoroughCare, it could create a warm handoff to one of its primary care or specialist practices.
Either during discharge or as the ambulatory practice picks up the transition of care, the patient can be enrolled in Remote Patient Monitoring. Needed devices can be ordered directly within ThoroughCare and delivered to the patient at home.
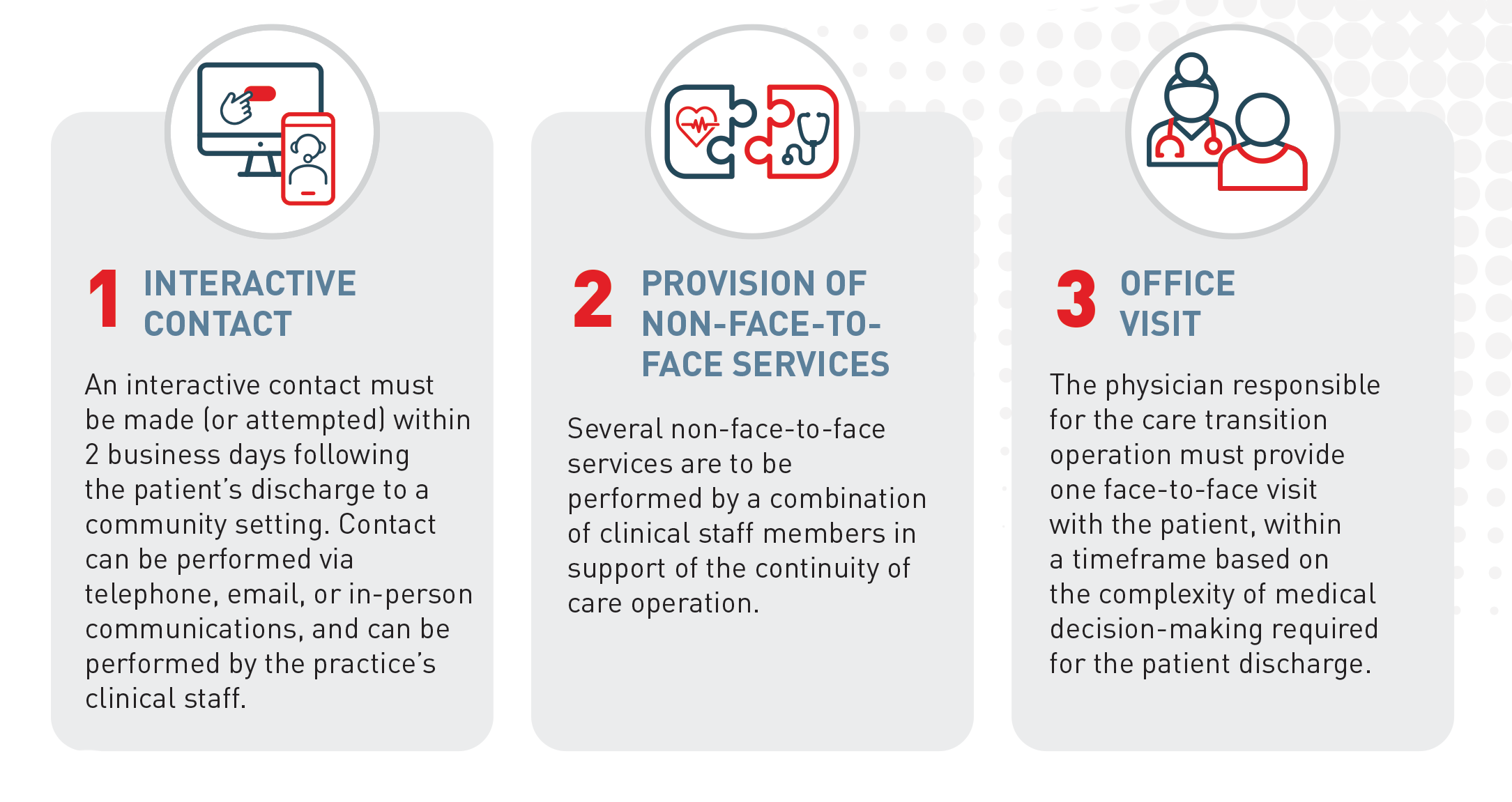
Because ThoroughCare is built upon evidence-based workflows and CMS rules for TCM, care managers and clinicians can seamlessly log and track time spent coordinating care for future billing. These workflow standards match TCM requirements (see Figure 2), enabling the care team to easily monitor and manage each patient’s 30-day transition deadlines.
Health systems that launch a TCM-RPM program through a hospital-ambulatory collaboration can look to reap the following four benefits.
Increase fee-for-service revenue
The Centers for Medicare & Medicaid Services (CMS) created several Medicare Part B care management programs that reimburse for time (and devices for RPM) for most providers (rural communities have different rules). Health systems can generate reliable, monthly fee-for-service revenue from these programs.
CPT code 99495 accounts for moderate-complexity TCM with a national average reimbursement rate of $203.34 per month per patient in 2024.
Reduce readmissions
TCM programs involving comprehensive discharge planning and follow-up have been shown to significantly reduce 30-day readmission rates. According to the American Journal of Medical Quality, patients decreased their odds of hospital readmission by nearly 87% when they participated in TCM.
This is particularly important if a hospital participates in the Hospital Readmissions Reduction Program, which is a value-based care purchasing program implemented by Medicare.
Improve quality measures and Star Ratings
Evidence demonstrates that RPM and TCM can significantly improve various quality metrics that contribute to Star Ratings. These improvements include:
- Better chronic disease management
- Reduced hospital readmissions
- Enhanced patient satisfaction
- Improved coordination of care
- Effective medication reconciliation to reduce medication errors
TCM programs that involve interdisciplinary teams improve care coordination, which enhances patient outcomes and satisfaction, both critical components of Star Ratings.
Additionally, structured follow-up care, including post-discharge phone calls and home visits, ensures continuity of care, improving health outcomes and patient satisfaction.
Lastly, TCM programs often focus on educating patients about their conditions and care plans, improving health literacy and self-management.
Enhance patient experience for chronic condition management and senior populations
Health systems with a large number of senior adults, patients living with one or more chronic conditions, or populations with potential complications (like hypertension in pregnancy) can benefit from a hybrid TCM-RPM program. When combined, these services provide intense and focused care coordination and monitoring during a high-risk time of transition from a high-acuity care setting to home.
RPM provides the real-time data needed for accurate oversight, and the Transitional Care Management approach provides timely interventions and follow-up to sustain health and avoid exacerbations or new problems. Plus, it ensures that patients and family caregivers are clear on the changes to the patient’s treatment and care plan after a hospital stay.
Through a seamless transition from hospital to home supported by team-based care and RPM, health systems can provide more comprehensive, reimbursable services and enhance patient experience, satisfaction, and loyalty throughout the healthcare journey.
Health systems can maximize impact and cash flow by combining TCM with RPM
Health systems can benefit from post-discharge Transitional Care Management and Remote Patient Monitoring by partnering with their ambulatory primary and specialty care providers.
Together, these programs can:
- Enhance the patient experience
- Provide continuity of care
- Reduce readmissions
- Provide a new revenue stream
ThoroughCare is a cloud-based care coordination platform that supports numerous care management programs, such as TCM and RPM, as well as Principal and Chronic Care Management and Behavioral Health Integration.


.jpg)
