Transitional Care Management: Rules, Requirements, and Benefits
30 days.
This is a critical time frame for patients with moderate or high-complexity medical issues after they have been discharged from an inpatient setting, such as a hospital.
During this period, chances of readmission are increased if proper transition and quality of care are not provided.
Transitional Care Management (TCM), a reimbursable, preventive wellness program, was started by the Centers for Medicare and Medicaid Services (CMS) to provide patients with such service.
Its goal is to eliminate gaps in patient care and reduce readmission rates.
Primary care doctors and specialists, as well as non-qualifying medical practitioners, can provide TCM services to patients.
The program can be applied upon discharge from one of the following settings:
- Inpatient acute care hospital
- Inpatient psychiatric hospital
- Long-term care hospital
- Nursing home
- Inpatient rehabilitation center
- Hospital outpatient observation/partial hospitalization
The result? Patients can see as high as an 86% decrease in odds of readmission compared with patients who did not receive TCM services.
Through our intuitive software, we’ve helped many clinicians deliver better quality care to their patients, including through the implementation of TCM. Below, we’ll expound upon the details of TCM and its benefits, and we'll put you on a path to starting your very own TCM program.
3 Required Components of Transitional Care Management
As discussed above, we know that TCM involves services provided to a moderate-to-high complexity patient within 30 days of discharge.
But what are those services?
There are three components of TCM that must be furnished.

1. Interactive Contact
Medicare requires interactive contact to be made with the beneficiary and/or caregiver, as appropriate, within 2 business days after the beneficiary’s discharge.
The contact can be made by telephone, email, or face-to-face.
The provider or clinical staff can make contact with the patient, provided they have the capacity for timely interactive communication in addressing patient status and needs.
For more information about interactive contacts, refer to the CPT Codebook available from the American Medical Association.
Medicare indicates that attempts to communicate should continue after the first two attempts in the required 2 business days until they are successful.
If you are unable to make contact after two or more separate attempts in a timely manner and document them in the medical record, you may report the service (provided that all other TCM criteria are met).
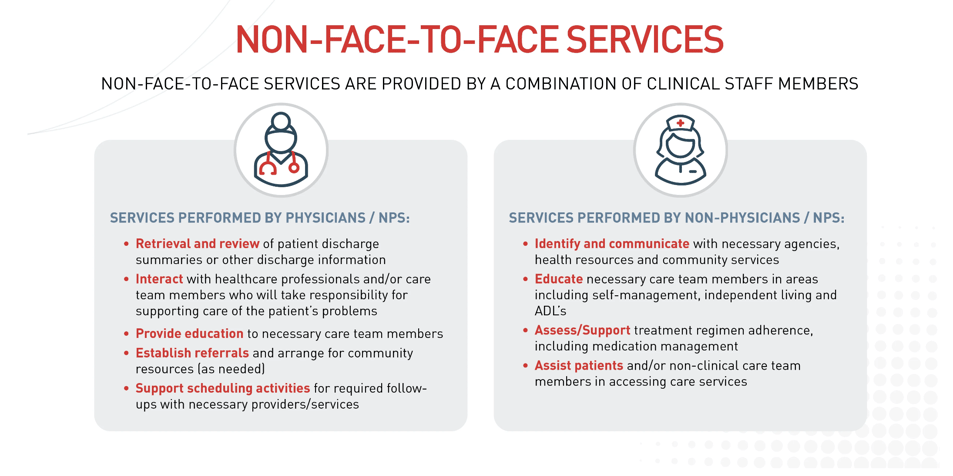
2. Non-Face-To-Face Services
Medicare requires the provision of non-face-to-face services to the patient unless you determine that they are not medically indicated or needed. Your clinical staff can also provide certain non-face-to-face services under your direction.
These include:
3. A Face-To-Face Visit
Finally, Medicare requires that you provide one face-to-face visit within certain timeframes. Medicare utilizes two Current Procedural Terminology (CPT) codes for billing. They are: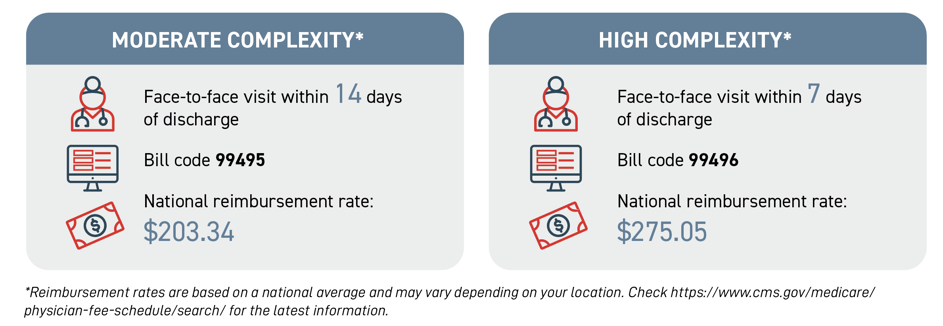 Please note: Face-to-face visits are part of the TCM service and should not be reported separately.
Please note: Face-to-face visits are part of the TCM service and should not be reported separately.
As you can see in the CPT codes above, the code you use depends on the level of medical decision-making.
Medical decision-making refers to the complexity of establishing a diagnosis and/or selecting a care management option, which is determined by the following factors:
- How many possible diagnoses and/or the amount of care management options need to be considered
- The breadth and/or complexity of medical records, diagnostic tests, and/or other information that needs to be acquired and analyzed
- The risk of significant complications, morbidity, and/or mortality as well as comorbidities associated with the patient’s presenting problem(s), the diagnostic procedure(s), and/or the possible management options
In order to qualify for a given type of medical decision-making, two of the three elements must either be met or exceeded.
4 Benefits of Transitional Care Management
While TCM is an excellent service that focuses on increasing the quality of health outcomes for patients, providers also stand to see a few benefits from providing such care.
1. Reduced Readmissions
As we mentioned earlier, the goal of TCM is to reduce the rate of readmissions and improve health outcomes for patients.
Hospital readmissions cost Medicare about $26 billion annually, with $17 billion spent on avoidable hospital trips after discharge. TCM can greatly reduce these costs to our healthcare system.
Additionally, Medicare has implemented value-based penalties for excessive 30-day hospital readmission rates. In 2017, Medicare penalized over 2,500 hospitals at a cost of more than $564 million for such excessive readmission rates.
By reducing readmissions, providers can reduce costs for themselves, Medicare, and their patients.
2. Higher Quality of Care
More and more, readmission rates are being used as a quality of care indicator.
Both commercial payers and consumers (patients) are using these rates to judge the quality of the provider.
A perceived lower value by patients can affect the bottom line of a practice.
3. Financial Reimbursement
As shown above, the national average for moderately complex care is $203.34 per patient per month, while the rate for high complexity is $275.05.
The financial incentives of TCM are clear.
When combined with the reduction in associated costs with readmissions and fewer hospital and office visits, providers stand to improve their bottom lines.
4. Chronic Care Management (CCM) Is Billable With TCM
Previously, Medicare would not reimburse for both Chronic Care Management (CCM) and TCM services in the same month. Now, it does.
This change allows for dual reimbursement for the same patient when “reasonable and necessary."
ThoroughCare Simplifies Transitional Care Management
ThoroughCare helps deliver integrated care management services to foster patient engagement and enhance revenue. Our platform provides the digital infrastructure to leverage fee-for-service programs while promoting value-based care objectives.
ThoroughCare supports end-to-end workflow for TCM, including:
- Tracking and reporting hospital discharges
- Coordinating time-sensitive transitional care services
- Simplifying reimbursement with automated CPT code assignment and an audit-proof record of care



