How do they work?
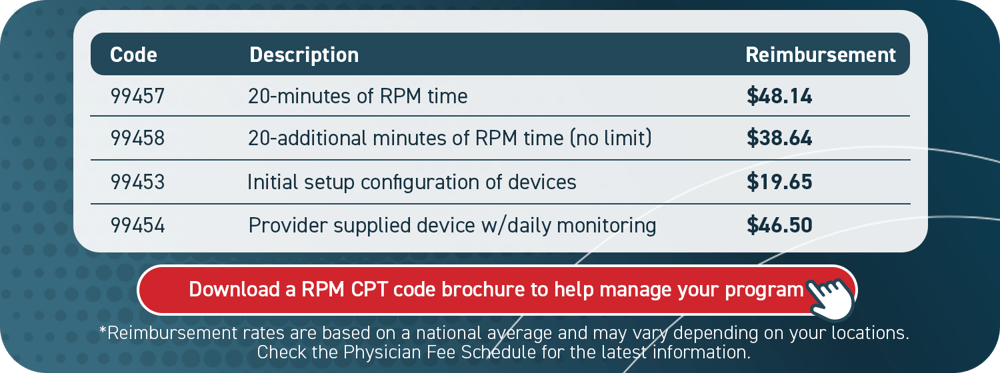
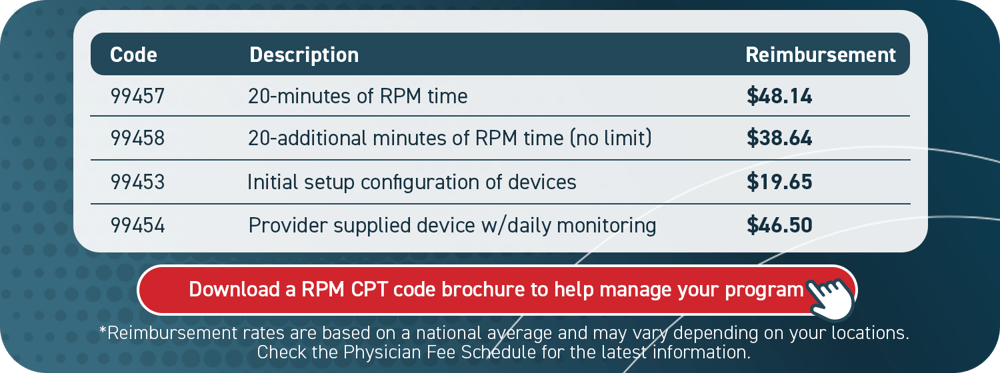
Remote monitoring CPT codes correspond to an exact activity, whether that be device setup or providing care services.
The codes reflect different rates, each with its own restrictions.
Providers, on average, receive $48.14 for 20 minutes of service per patient per month (99457). Additional opportunities to meet higher billing thresholds are also available. For example, an additional $46.50 per month is billable when patients utilize their RPM device daily (99454).
Best practices
- CPT code 99453 (device setup): This can be claimed only once per device, and it cannot be billed more than once per month per patient. For example, if a patient receives two devices within the same calendar month, only one device can be billed for in that timeframe. The second device would be billable in the subsequent month.
- CPT code 99454 (device use): This can be claimed once per month per patient, no matter the number of devices employed by that patient. It should be billed in 30-day increments only if the patient takes at least 16 daily device readings that same month. These readings do not need to be taken on consecutive days.
It is important to note: CPT code 99454 (device use) can be billed every 30 days while codes 99457 and 99458 (program time) are calendar month codes. Aligning claims submissions for these codes is recommended.
We would suggest submitting all RPM-related claims together by calendar month.