Remote Patient Monitoring (RPM)
The Best Use Cases for Remote Patient Monitoring
What does it take to create an effective and profitable Remote Patient Monitoring program?
Creating the best Remote Patient Monitoring use cases considers four factors:
- The provider setting
- Which medical conditions need monitoring
- The technical capabilities of the patient population
- The type of RPM device required
In addition to these four components, each organization must consider how it will manage the program and its data. This is where ThoroughCare plays a critical role.
Built as a foundational care management platform, ThoroughCare provides an end-to-end solution for Remote Patient Monitoring. The software enables clinical teams to manage chronic conditions through measurements taken by patients via Internet- or cellular-connected devices.
Four Remote Patient Monitoring use case components
Remote Patient Monitoring (RPM) is a telehealth program covered by Medicare Part B created to enhance chronic condition management.
While RPM can be used in various care models and has varying levels of coverage by commercial insurance, this program focuses on seniors with chronic conditions who could benefit from regular or continuous monitoring at home.
Whether as a standalone program, or in combination with Chronic Care Management or Transitional Care Management, RPM gives providers physiological data to enhance chronic disease management.
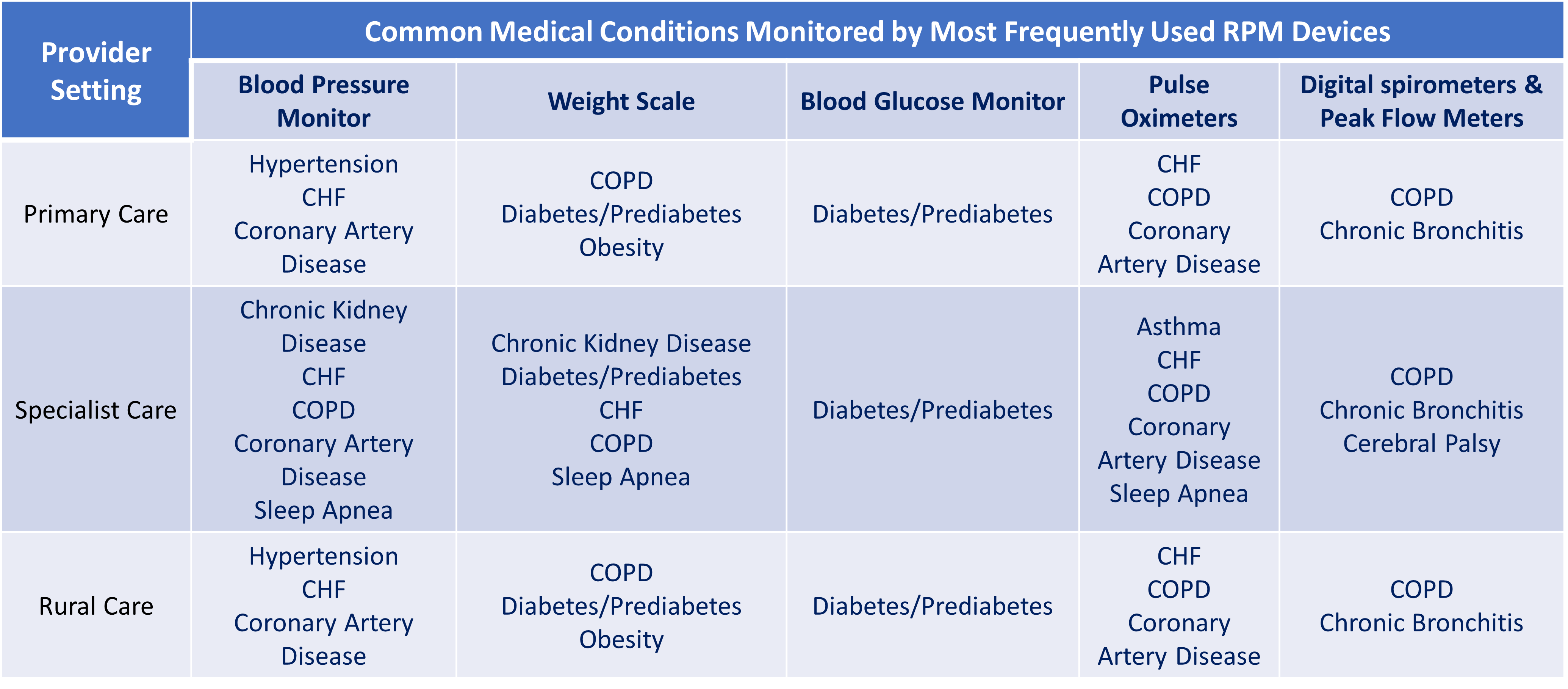
Figure 1 highlights example use cases for RPM across provider settings, commonly monitored medical conditions, and the most frequently used RPM devices.
Let’s look at each component as building blocks to create the best RPM program for your healthcare organization.
Provider settings
Primary care providers, rural physicians, and physicians across multiple specialties use patient physiologic data to achieve three goals:
- Gain adequate chronic condition control
- Avoid clinical exacerbations
- Monitor a patient’s progress and adherence to their care plan
In the primary care setting, RPM helps clinical teams monitor high-risk patients between visits for the most common chronic conditions, such as diabetes and hypertension. When paired with care management programs, primary care practices can create an additional revenue stream while providing continuous and ongoing care.
In the specialist care setting, RPM devices can target specific conditions and clinical measures. RPM data provides an early detection alert when a patient’s clinical picture worsens, but symptoms haven’t surfaced yet.
In the rural care setting, RPM helps to fill the gap of reduced access to care. Research demonstrates RPM’s efficacy in rural settings, particularly for diabetes, heart failure, and chronic obstructive pulmonary disease (COPD).
One study at Mayo Clinic found that 72.5% of RPM patients complied more closely with their care plan tasks, such as taking medication and monitoring vitals. Only 9.4% of the RPM patients were readmitted within 30 days, compared to 20% of patients not using RPM.
Across various care settings, RPM has been shown to help providers improve patient self-care, create more efficient communication, and increase patient confidence and patient education.
Medical conditions
There are many symptoms and conditions that the Health Resources and Services Administrations say can be tracked with Remote Patient Monitoring as a subset of telehealth, including:
- High blood pressure
- Diabetes
- Weight loss or gain
- Heart conditions
- COPD
- Sleep apnea
- Asthma
Some of these chronic conditions are highlighted in high-quality research.
Hypertension is a keystone medical condition leading to many other diseases. RPM is effective in helping patients lower their blood pressure, follow treatment plans, adhere to medication regimens, and self-manage.
A study by the GAO3 (US Government Accountability Office) reported that provider and patient associations found RPM to be a significant contributor to improved or maintained quality of care. RPM use was also associated with substantial reductions in mortality and hospitalization in cardiovascular-related conditions.
Other studies showed that Remote Patient Monitoring helped providers and patients better manage diseases like COPD and congestive heart failure, resulting in fewer emergency department visits, hospital readmission avoidance, and reduced hospital length of stay.
Beyond these most commonly monitored conditions, RPM is being tested upon discharge for conditions like cirrhosis, acute kidney injury (AKI), post-pancrectomy, and post-gastroenterology procedures.
Systematic research reviews of high-quality studies on RPM found that Remote Patient Monitoring could positively impact conditions like Parkinson’s disease, low back pain, fall detection and mobility-related diseases, and neurological and brain disorders.
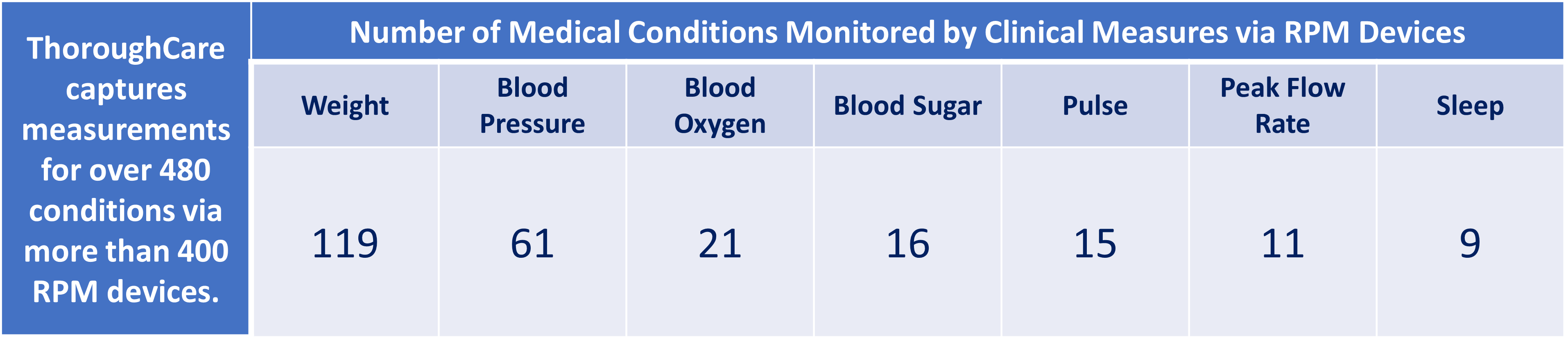
As highlighted in Figure 2, ThoroughCare connects to more than 400 RPM devices and tracks data for clinical measures necessary to monitor over 480 medical conditions. The matrix shows the number of diseases ThoroughCare can monitor via the most common measures.
Patient population
There are four requirements for a patient to be eligible for Medicare’s RPM program. These are:
- A patient must have an acute or chronic condition
- This condition must pose a risk of death, acute decompensation, or functional decline
- The condition must be noted by the provider 12 months prior to enrollment
- A patient must have an established relationship with their provider
In addition to these requirements, and looking at your patients' health needs and risk profile, launching an effective RPM program considers patients’ technical capabilities, cellular or Internet connectivity, and any other barriers that might make one RPM device better or easier to use.
There are two device connectivity options —cellular devices and Bluetooth® devices that rely on cellular service. Your patient’s geographical location, carrier, or Internet service may affect their RPM participation.
Other factors to consider are potential barriers to patient use and adoption, including:
- Patient’s technical ability and your desire to provide needed support
- The specific RPM device and how easy or complex it may be to use
- Cellular RPM devices tend to be easier to use out of the box
- Bluetooth can be more challenging because of the need for regular updates and pairing
Remote Patient Monitoring devices
The technology side of creating an RPM program may seem the most daunting. However, ThoroughCare enables end-to-end operational, technical, and clinical data management across all patients and devices.
ThoroughCare can integrate with more than 400 RPM devices that collect weight, blood pressure, blood glucose, oxygen saturation, temperature, respiratory rate, sleep, heart rate, and many more clinical measures.
We offer the most popular and proven Remote Patient Monitoring devices through our partners, such as BlackBox RPM, BodyTrace, Dexcom, SmartMeter, and Tenovi. We also work with Validic to ensure access to more than 400 additional RPM device brands.
Whether you’re looking to manage one or two of the most prevalent chronic conditions with the most frequently used RPM devices, or you want help in choosing the best FDA-approved devices that are easiest for your patients to use, our clinical and technical teams are here to help.
ThoroughCare simplifies Remote Patient Monitoring
ThoroughCare ensures your RPM program meets Medicare’s requirements, facilitates data collection and analysis, and enables personalized care planning.
Additionally, our platform helps:
- Enroll new RPM patient participants
- Order, register, and manage RPM devices
- Coordinate device set up on behalf of patients to ensure effective care management
- Meet enrollment and tracking requirements for RPM devices and time allotments
- Bill Remote Patient Monitoring CPT codes, including 99453, 99454, 99457, and 99458
- Automate device- and time-based claims documentation for auditing
- Assess patient symptoms, condition barriers, and care goals to determine planned interventions and expected outcomes
- Alert care teams when RPM data is outside set patient parameters



