Chronic Care Management | Remote Patient Monitoring (RPM)
How Chronic Care Management Works with Remote Patient Monitoring
Combining Chronic Care Management with Remote Patient Monitoring can improve clinical outcomes, lower total cost of care, and enhance patient satisfaction.
Here, we’ll provide guidance on how a provider organization can offer and bill for a combined program while confidently complying with Medicare’s requirements.
Synergies of Chronic Care Management and Remote Patient Monitoring
Chronic Care Management and Remote Patient Monitoring make a powerful diagnostic-therapeutic combination.
The CCM program offers comprehensive care and goal planning, as well as ongoing patient support and education. RPM leverages wearable and at-home devices to monitor patient's physiologic data, sharing the results directly with healthcare providers in real-time.
Figure 1 shows where CCM and RPM aspects overlap. When the value of both programs is combined, providers have regular, robust patient-generated data that gives them insight into the patient’s status. This enables the care team to take action and intervene earlier, thereby mitigating risk or avoiding exacerbation.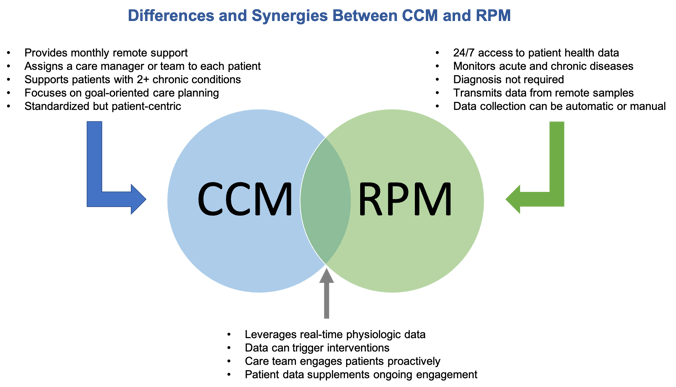
Adding Remote Patient Monitoring to an existing Chronic Care Management program can also yield other benefits.
A systematic research review found that, for all disease conditions, RPM was reported to reduce admissions, length of stay, and emergency department presentations in nearly 50% of studies. RPM was particularly effective for chronic obstructive pulmonary disease (COPD) at reducing emergency presentation.
Evidence from a health economic perspective shows that RPM is beneficial for chronic disease management. Compared with traditional care, RPM was highly cost-effective for hypertension in preventing high-cost health events.
Remote Patient Monitoring supports continuously managing chronic disease for patients in the comfort of their homes. Additionally, research has shown that it can deliver an excellent overall patient experience.
One large study found that RPM program participants had a high level of satisfaction:
- 93.58% were satisfied with the RPM program and ready to graduate when meeting the program goals
- 92.76% had confidence in RPM and would recommend it to people with similar conditions
- 88.97% agreed or strongly agreed that the RPM program helped them feel comfortable managing their health from home
Lastly, RPM can be used as a strategic tool toward CCM goals. When combined with a holistic, person-centered approach to chronic disease management, the duo helps close gaps between in-person appointments and telephonic touchpoints.
CCM and RPM, when combined, can provide a sense of comfort to patients that they are being monitored at a distance.
Offering and billing CCM and RPM concurrently
The Centers for Medicare & Medicaid Services (CMS) acknowledges the complementary nature of Chronic Care Management and Remote Patient Monitoring by allowing concurrent billing between the two programs.
RPM can be delivered as a standalone program or alongside programs like CCM, Transitional Care Management, Behavioral Health Integration, and Principal Care Management.
CCM and RPM can be billed concurrently with caveats
While CMS permits concurrent billing of RPM with programs like CCM, there are several primary billing rules to keep in mind:
- Minute double-counting is not allowed. If activity minutes are accrued and submitted for one program or CPT code, they cannot be used again under a different CPT code.
- Providers must collect at least 16 days of data per 30-day period to bill for device use based code 99454. For time-based billing, providers should offer at least 20 minutes of clinical engagement to bill for code 99457.
- RPM can only be offered to established patients, including those who have been evaluated and have a treatment plan.
- RPM services can only be billed under one practitioner, even if they use more than one RPM device.
Each program must meet independent requirements
While CCM and RPM can be billed concurrently, the provider organization must still meet each program’s individual billing requirements and document compliance appropriately. The following charts outline the CPT codes and main requirements for both programs. These codes pertain to fee-for-service (FFS) Medicare programs offered by non-rural provider organizations.
Chronic Care Management
Remote Patient Monitoring
CCM and RPM for rural health provider organizations
Rural healthcare organizations—including federally qualified health centers (FQHCs) and rural health centers (RHCs)—have billing criteria different from those of FFS providers.
New for 2024, CMS permits RHCs and FQHCs to bill for Remote Patient Monitoring.
While other providers have numerous codes for billing various care management programs, rural health organizations have one HCPCS code, G0511, to cover all available programs.
The 2024 Physician Fee Schedule Final Rule expanded the codes that could be reimbursed under G0511 to 28, which includes RPM and CCM (non-complex, complex, and physician-delivered).
Under the G0511 code, rural providers can bill for more than one instance monthly for different care management services.
However, the 2024 Final Rule did not establish a maximum number of times the code could be filled in a given month. More clarification is needed from CMS on whether billing more than once per month per program is allowed.
Read this article to understand the best practices for using G0511 for CCM and RPM
ThoroughCare simplifies CCM and RPM
ThoroughCare is a comprehensive software platform that supports end-to-end workflow and simplified billing for Chronic Care Management and Remote Patient Monitoring. ThoroughCare provides a structured approach to care management while enabling flexibility to meet individual patient needs. This includes:
- Enrolling new patient participants in CCM and RPM
- Creating and maintaining comprehensive patient care plans
- Ordering, registering, and managing RPM devices
- Coordinating device set-up on behalf of patients to ensure effective care management
- Meeting enrollment and tracking program requirements
- Automating device- and time-based claims documentation for auditing
- Assessing patient symptoms, condition barriers, and care goals to determine planned interventions
- Alerting care teams when RPM data is outside set patient parameters


.jpg)
.png?width=1500&height=660&name=unnamed%20(13).png)
.png?width=1500&height=560&name=unnamed%20(14).png)
