Care Coordination | Patient Engagement | Care Management
What is a Patient-centered Care Plan?
Many physicians and clinicians pride themselves on the relationships they develop with their patients. By creating a patient-centered care plan, providers can enhance engagement, deliver timely interventions, align on outcome goals, and improve care team coordination.
At its most broad, a care plan is a living document that captures a patient’s current health information and conditions. It outlines treatments, care services, and goals the provider will help patients receive or address.
A “patient-centered” care plan considers the person’s individual needs, and it is created in collaboration with them. The patient is the owner of this document, but it can be shared between care team stakeholders, as well as family members, based on their consent.
A patient-centered care plan differs from a standardized one, which is already pre-developed to specific conditions and does not consider the person’s exact needs. Clinical teams, including nurses or care managers, can use the patient’s individualized plan of care to coordinate activities and services. This can help prevent duplicative efforts, promote patient data sharing, and potentially cut costs.
Care planning can involve ongoing conversations and engagement with patients, beyond the initial plan development. Once a care plan is created, whether for general coordination of services or a specific program, it is revisited regularly to:
- Ensure interventions and services align to patient goals and desired outcomes
- All current and accurate health information is captured
- Updates are made based on condition needs or ongoing management
As chronic disease management, value-based care, and integrated behavioral health become more of a focus for primary care, ensuring that all services are patient-oriented and can support better outcomes and improve patient and provider satisfaction.
Common features of patient-centered care plans
Though each patient-centered plan of care is unique to the individual, all should support the following:
1. Collaboration and coordination
The care a patient receives is most effective when it is collaborative, coordinated, and accessible. For instance, a study published by the Journal of the American Medical Association found that the inability to coordinate care effectively accounts for $29.6 billion to $38.2 billion in wasted healthcare spending per year.
An individual care plan should focus on making the patient journey seamless. It should support clinicians in aligning front-line patient care, clinical care, and ancillary and support services. This is crucial to:
- Reducing fragmentation or duplication of services and tests
- Improving patient satisfaction and engagement
- Enabling more holistic, person-centric care to improve outcomes
To create an effective care plan that reflects these priorities, providers should tap into their intimate rapport and relationship with patients to become partners. Active collaboration and shared decision-making among patients, families, and providers are key.
Specially, with patients, making them feel part of a collaborative process is important to help motivate self-care and management, as well as enable measurable progress on specific goals.
2. Physical and emotional care
Under the patient-centered care model, both physical and emotional care is provided. Physical care is provided through pain management, assistance with activities and daily living needs, and even the environment in which the care is provided.
Care plans can help address these needs by:
- Accounting for current medications or interventions and implementing others
- Educating patients about their specific conditions and how best to live with them
- Supporting behavioral and lifestyle changes through proactive goal setting
- Assessing social determinants of health (SDOH) to identify barriers to care and potential needs for community support or other resources
Emotional care can help treat a patient’s anxiety in dealing with chronic illnesses, physical limitations and treatment effects, as well as its impact on their family and lifestyle.
Results from evidence-based assessments, such as PHQ-9 (Depression), GAD-7 (Anxiety), or MDQ (Mood Disorders), can help patients and clinicians further tailor care plans for emotional needs, or identify gaps in care.
3. Involvement of informal caregivers and community supports
Home and community-based family and friends are an essential part of the patient-centered care model.
Including them in the patient’s care and planning adds another layer of support both physically and emotionally while also giving physicians an advocate in the home.
Providers can involve additional stakeholders by:
- Including the patient’s family or support network in all care discussions. They can help the patient understand concerns or know what their health plan offers, or provide caregivers with additional medical history.
- Educating family members or supporting individuals alongside the patient. They may also be unfamiliar with specific health effects from conditions or how certain medications work.
- Considering the patient’s values. Speak to family members and approach goal setting with your full understanding of the patient. Also consider possible language barriers, health literacy issues, and other SDOH factors.
Often, a family member or friend can help motivate, educate, and engage the patient, as well as ease patient concerns.
Care plans that are created through a digital platform can often be easily shared with key stakeholders, promoting greater accessibility.
4. Continuity in treatment
Care management programs facilitate ongoing monitoring, education, and intervention. Care can continue through regular touchpoints between in-person visits, supporting the patient’s progress, care plan adherence and lifestyle choices.
One example is Chronic Care Management (CCM). A Medicare Part-B program for patients with two or more chronic conditions, clinical staff can use this service to engage patients for at least 20 minutes per month and coordinate care activities.
Studies have shown that CCM programs can reduce hospital admissions and cut health costs in the long term.
Along with supporting care plan use for patients, a Chronic Care Management program also includes:
- A monthly clinical review
- Telephone check-ins
- Physician reviews
- Referrals
- Prescription refills
- Chart reviews
- Scheduling appointments or services
5. Transparency and knowledge
Physicians build positive patient relationships by being upfront and honest. That transparency helps when working with patients to manage chronic illnesses or complex clinical scenarios.
Creating a patient-centered care plan leverages that transparency when it comes to setting goals, gaining commitment to healthier behaviors, and educating patients on self-management techniques. Not only does this enhance quality and safety performance but it builds patient confidence in managing their own health.
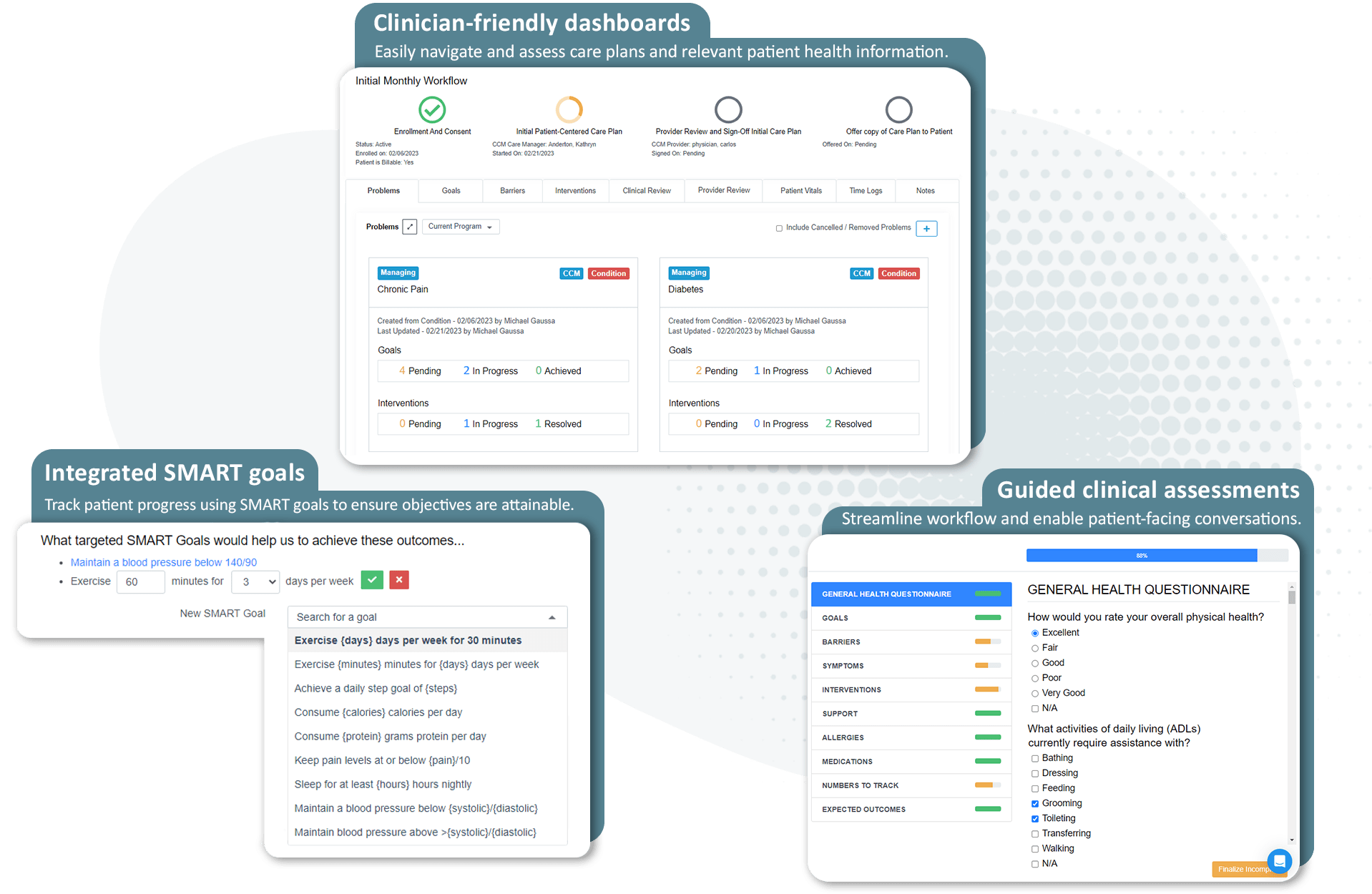
Standardized care plans: ThoroughCare helps providers engage patients in evidence-based care planning
ThoroughCare is a comprehensive platform that helps providers streamline care coordination and management.
How a plan of care benefits patients
Beyond the trust developed with a physician and their care team, a patient-centered care model offers many benefits to patients that also, ultimately, benefit healthcare providers.
1. Improved experience and satisfaction
Providing a beneficial patient experience is its own goal. However, according to the Agency for Healthcare Research and Quality, “substantial evidence points to a positive association between various aspects of patient experience, such as good communication between providers and patients, and several important healthcare processes and outcomes.”
These can include:
- Improved patient safety practices
- Less use of unnecessary services
- Adherence to medical advice
Involving patients in the decision-making process of their care also makes them feel valued and empowered. A patient-centered care plan puts the patient in the driver’s seat as it addresses their individual needs, preferences, and unique values.
By taking a collaborative approach to the patient’s healthcare and respecting their needs, their overall experience is improved and satisfaction scores tend to respond.
2. Proactive, collaborative engagement
Within primary care, the patient-centered care model aims to fully inform someone about their health. This includes the full scope of their conditions, their prognosis, and the actions patients and providers can take to improve care.
Any success depends, however, on engaging patients in effective, measurable ways that improve outcomes. The plan of care can serve as a recurring touchpoint to connect the patient with their care manager or nurse.
Through these regular meetings, a clinician can use health information captured within the care plan to personalize engagement and monitor progress on certain outcomes. Care plans can also leverage motivational interviewing techniques to help patients act toward greater self-management.
3. A focus on better health outcomes
Preventive healthcare is generally considered an effective way to identify health risks earlier. This can help providers address certain conditions before they cause others.
Patient-centered care plans facilitate a regimen of standard preventive care services, including screenings, vaccines, and medication review. This can also have a positive impact on any present conditions.
According to the British Journal of General Practice, care planning has been shown to “improve patients’ confidence and skills in self-management. There is evidence that among engaged patients it can improve health outcomes.”
How a patient-centered care plan benefits providers
While a patient-centered care model focuses on improving an individual’s health outcomes, the benefits afforded to the physician and the larger care organization are numerous.
1. Improved patient satisfaction
By improving your patient’s health and experience, your practice will see improved satisfaction scores among patients and their families.
These scores can boost the practice’s reputation, supporting loyalty and word-of-mouth that leads to growth and revenue.
Patient experience surveys, such as the Consumer Assessment of Healthcare Providers & Systems (CAHPS), account for standardized measures related to satisfaction. They can also impact provider payment under specific value-based care contracts.
2. Greater care team experience and loyalty
One of the biggest reasons people choose to work in the healthcare industry is that they want to help people. The relationships between staff and patients are at the core of the patient-centered care model.
As a practice provides improved quality of care and realizes higher levels of patient satisfaction, the employee experience improves as well. A happier, more engaged care team supports greater productivity and quality performance.
3. Increased revenue and growth
While many benefits may be intangible or downstream, practices can see an impact on their bottom line through:
- Increased efficiencies
- Improved resource allocations
- New revenue streams
- New opportunities from value-based care contracting
Care management programs that rely on care planning also support fee-for-service reimbursement. Providers can use this revenue to hire and expand care teams to address quality performance goals.
4. Alignment with value-based care objectives
As mentioned above, care planning can help improve patient satisfaction surveys. But beyond this one measure, plans of care enable a personalized approach that is key to implementing value-based care.
Delivering streamlined care management and team-based coordinated care—coupled with a patient-centered approach—help practices become more efficient, enhance quality and care outcomes, and transition to more risk-based arrangements.
Chronic Care Management programs that utilize patient-centered planning can give providers a standard workflow to hit value-based metrics.
How to create and update a plan of care
A care plan created as part of comprehensive care management should include the following five elements:
- Systematic assessment of the patient’s medical, functional, and psychosocial needs
- System-based approaches to ensure timely receipt of all recommended preventive care services
- Medication reconciliation with review of adherence and potential interactions
- Oversight of patient self-management of medications
- Coordinating care with home- and community-based clinical service providers
Once a patient is enrolled in a care management program and medical or behavioral conditions have been identified and prioritized, it’s time to lay the foundation for improved health through collaboration, coaching, and healthy actions.
Creating a care plan involves talking to the patient and collecting personal information and health data. This process can be facilitated through questionnaires or guided interviews. Data can include:
- Medical history and personal details
- Emergency contacts
- Information specific to any existing chronic conditions and related medications
- Desired outcomes and goals
- Health plan coverage
- Broader care team information to assist with coordination of services
While there isn’t one specific way to create a care plan, there are general best practices providers can follow. These can be critical talking points that ensure the most effective plan of care is developed. These can include defining the patient’s goals, identifying barriers to achieving them, and deciding which metrics to track.
Defining SMART goals through care planning
SMART goals have been demonstrated to help patients create healthier habits. They establish clear, internally-motivating, and measurable targets that align to the person’s desired outcomes. By using the care planning process, nurses can work with patients to identify where these opportunities might be.
Care managers can also create action plans to give patients a feasible, step-by-step method to integrate their goals into daily life. Together, the patient and provider can consider the circumstances that might disrupt progress. This exercise can help develop other options for when barriers emerge.
Evidence supports the effectiveness of SMART goal-setting in healthcare.
An analysis by the U.S. Preventive Services Task Force on SMART goal efficacy found they effectively reduced weight or improved eating behavior in 65% of studies. The Journal of Pharmacy Practice found that patients who set SMART goals lowered their A1c.
Identifying gaps in care
Care managers can use the patient’s plan to review any preventive services or upcoming screenings that are due and address any care gaps. Left ignored, these gaps lead to further complications in health, such as late or missed diagnosis or comorbidities.
How ThoroughCare creates patient-centered care plans
Our platform provides evidence-based assessments, education, and workflows to enable a patient-centered care planning approach. We give nurses and care managers the tools to take all necessary steps required by CMS for care management delivery.
Featuring clinical content based on recommendations from the American Academy of Family Physicians, our guided interview walks care managers and nurses through a patient-centered care plan, providing the most common questions and answers to effectively identify, manage, and treat every patient’s chronic conditions.
Additionally, ThoroughCare can help clinicians:
- Help motivate patients through clinical recommendations
- Analyze patient risk factors and generate clinical recommendations
- Identify behavioral health conditions
- Track and log services for an audit-proof record of care