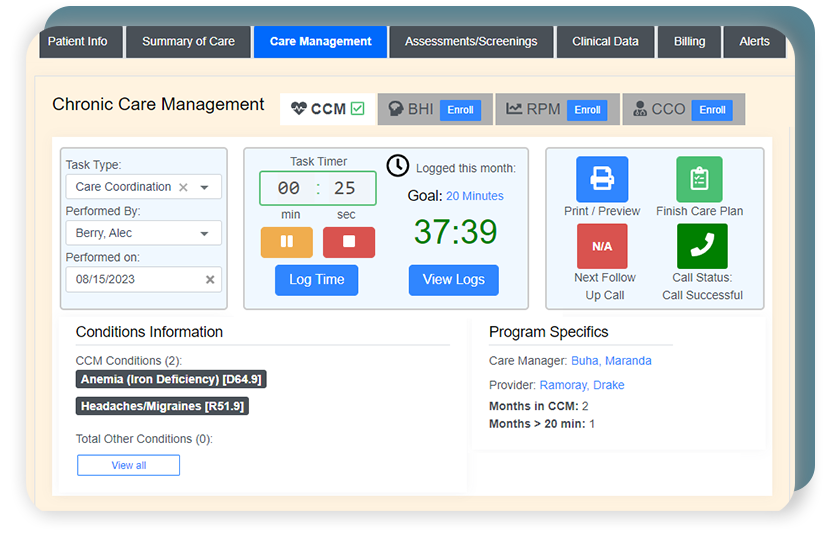
Different CPT billing codes reflect specific categories of CCM. The qualifying determinants are who provides program services, complexity of medical decision-making, and the length of time spent with the patient.
CPT codes 99490 and 99439 for non-complex CCM
Billing code assignment is based on the complexity of medical decision-making.
As shown in the graphic above, CCM billing codes specify Complex and Non-complex chronic care services. Within these categories, codes further reflect different lengths of time spent with patients and the level of physician involvement required.
In some instances, Non-complex CCM can be provided by clinical staff.
For Non-complex CCM, the following CPT codes can be used to account for reimbursement based on all program requirements being fulfilled.
- CPT code 99490 for 20 minutes of billable time
- CPT codes 99490 + 99439 for 40 minutes of billable time
- CPT codes 99490 + 99439 (x2) for 60 minutes of billable time
Two ICD-10s must be presented when billing for chronic care services as the requirement for CCM includes two or more present conditions.
CPT codes 99491 and 99437 for physician-driven, non-complex CCM
The following codes are designed for non-complex chronic care in which the provider or non-physician practitioner (NPP) is heavily involved. They cannot be billed concurrently with standard CCM CPT codes (reviewed in the prior section).
The value of physicians’ time is reflected in these non-complex, physician-driven codes as CCM services are not reliant on clinical staff:
- CPT code 99491 for 30 minutes of billable time
- CPT codes 99491 + 99437 for 60 minutes of billable time
CPT codes 99487 and 99489 for complex CCM
The following billing codes apply for complex care:
- CPT code 99487 for 60 minutes of billable time
- CPT codes 99487 + 99489 for 90 minutes of billable time
It is important to note the distinction between CPT code 99487, which accounts for 60 minutes of complex chronic care, versus the two CPT codes (99491 and 99437) that account for 60 minutes of physician-driven, non-complex chronic care.
In the case of a Medicare audit, you will want to show the correct code was applied based on the compatible situation.