Care Coordination | Patient Engagement | Care Management
How Nurses Can Create and Update a Patient’s Care Plan: An Example
As a nurse or clinician, creating and updating a care plan is crucial to effectively coordinating patient services and interventions, and overseeing medication management.
Care planning is also a core activity for reimbursable Medicare services, such as Chronic Care Management (CCM), Principal Care Management (PCM), and Behavioral Health Integration (BHI).
A patient-centered care plan is most effective when it’s based on a physical, behavioral, cognitive, psychosocial, functional, and environmental assessments or reassessment.
A comprehensive plan identifies and prioritizes health issues, paying particular attention to any comorbidities and chronic conditions.
As the foundation of care coordination, how can clinicians and nurses ensure they create effective patient-centered care plans? And, what does CMS require for care plans used in care management programs? What monthly updates must be made?
What should nurses consider for a care plan?
A care plan created as part of comprehensive care management should include the following five elements:
- Systematic assessment of the patient’s medical, functional, and psychosocial needs
- System-based approaches to ensure timely receipt of all recommended preventive care services
- Medication reconciliation with review of adherence and potential interactions
- Oversight of patient self-management of medications
- Coordinating care with home- and community-based clinical service providers
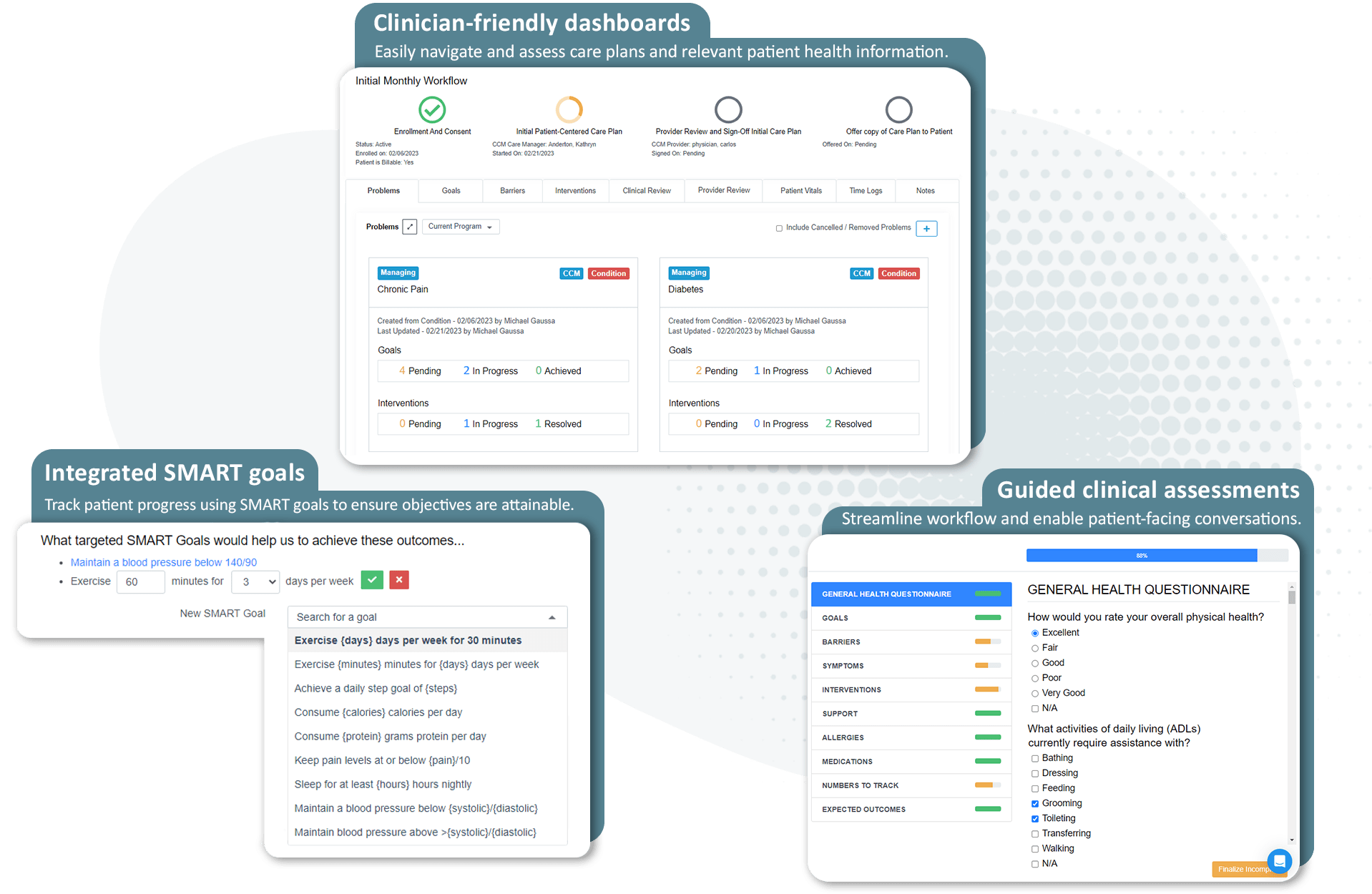
Standardized care plans: ThoroughCare helps nurses engage patients in evidence-based care planning
ThoroughCare is a comprehensive platform that helps providers streamline care coordination and management.
8 steps to create a care plan: an example
Once a patient is enrolled in a care management program and medical or behavioral conditions have been identified and prioritized, it’s time to lay the foundation for improved health through collaboration, coaching, and healthy actions.
#1 Defining the patient’s goals
The first step in creating a care plan includes identifying and solidifying the patient’s goals.
Because goals are measurable and can be tracked and updated over time, they give patients, care teams, and providers focus.
For example, if the patient’s condition is hypertension and their goal is to participate in more physical activities with their grandchildren, the nurse can focus on common activities that support their success, including:
- Lower blood pressure
- Stay on a low-salt eating plan
- Exercise more regularly
- Maintain healthy kidney labs
When patient goals are data-driven, the goals focus on metrics that have clear ranges. Within these boundaries, care teams can regularly reevaluate and intervene.
Clearly defined goals drive accountability and transparency between nurses or care managers and their patients, giving both a way to track progress and change tasks or tactics if progress stalls.
#2 Identify barriers to achieving care plan goals
Identifying potential roadblocks to patients reaching their goals is critical to anticipating obstacles and determining if-then actions.
Continuing with the hypertension condition used above, the patient may face common barriers, including:
- Food doesn't taste good without salt
- Not knowing how to read food labels to check sodium amounts
- Lack of energy or motivation to exercise
- No home blood pressure monitor
- Needs instructions to use home blood pressure monitor
#3 Identify patient symptoms
Discuss and uncover the symptoms the patient has been experiencing for the conditions you’ve identified.
For hypertension, the patient may be experiencing symptoms like a pounding heartbeat, headache, flushing or feeling hot, and other hypertension-related symptoms.
#4 List potential clinical interventions
Interventions are actions the nurse or care manager takes toward achieving patient goals and realizing desired outcomes. Common interventions include:
- Patient education
- Self-management coaching
- Reviewing medications and purpose
- Checking vital signs
- Assessing the patient’s pain levels
Related to hypertension, some common interventions could include:
- Teaching the patient what is occurring in the heart during systole and diastole
- Reviewing goal blood pressure levels set for the patient by their provider
- Teaching the patient the possible health outcomes if blood pressure remains high: stroke, heart attack, kidney disease, vision loss, etc.
- Educating the patient in the goal sodium level set by the provider
- Educating the patient on the role a high sodium level plays in increasing blood pressure
- Teaching the patient how to read a food label to check the sodium levels of the foods they eat
- Educating the patient on the lifestyle changes that help to decrease blood pressure, such as a daily exercise routine
- Teaching the patient the important role medications play in controlling blood pressure
#5 Document the complete patient care team
It's extremely important to have an accurate list of all providers involved in the patient’s health care. Active collaboration and shared decision-making between patients, families, and providers are key to a successful patient-centered care plan.
Make a list of everyone involved in the patient’s health, including contact information.
#6 Identify patient allergies and medications
Ensure that any prescribed new treatment won’t trigger allergies or be contraindicated with their medications. If the patient’s clinical picture is complex, engage a pharmacist for review.
#7 Decide which metrics to track
First, determine which patient vitals are primary, which may include weight, BMI, and blood pressure.
Next, identify needed lab work. For a patient with hypertension, consider tracking lab results like HgbA1C, LDL cholesterol, HDL cholesterol, total cholesterol levels, INR (if on Warfarin), and Triglyceride levels.
#8 Regularly monitor expected outcomes from treatment
Expected outcomes are similar to goals but take a broader view of what the patient looks forward to seeing more or less in a future state.
For a patient with hypertension, expected outcomes could include:
- Less worry that their blood pressure is high
- Less worry about having a stroke or heart attack
- Less worry about their kidney function
- Increased confidence in taking their blood pressure at home
- Less reliance on medications
- Feel more motivated to increase activity
These steps ensure that a nurse or care manager has created a holistic, patient-centered care plan. Armed with this foundational tool, the care team can spend more time on patient engagement and education with a focus on goal-oriented action.
Once established, the care plan should be updated monthly.
How are care plans updated?
CMS requires providers to update the patient care plan monthly with any relevant information.
Care plans should be written to enable systematic assessment on a month-to-month basis, noting changes, improvements, or interventions needed, accounting for specific patient health problems.
For example, each month, the care manager should review the medication list and any associated problems and, if necessary, inform the physician of new issues or needs.
Using the initial care plan as a baseline, the care manager can discuss and document any relevant issues or concerns in regard to the patient’s health.
The update should include any actions the patient is taking to address those issues to ensure progress is being made toward their goals.
Additionally, the care manager should review any preventive services or upcoming screenings that are due and address any care gaps. Once discussed, the care manager can order needed services.
While CMS doesn’t provide details on what they look for in care plan updates, these steps ensure the care plan is current.
How ThoroughCare streamlines care plan creation
Our platform provides evidence-based assessments, education, and workflows to enable a patient-centered care planning approach. We give nurses and care managers the tools to take all necessary steps required by CMS for care management delivery.
Featuring clinical content based on recommendations from the American Academy of Family Physicians, our guided interview walks care managers and nurses through a patient-centered care plan, providing the most common questions and answers to effectively identify, manage, and treat every patient’s chronic conditions.
Additionally, ThoroughCare can help clinicians:
- Help motivate patients through clinical recommendations
- Analyze patient risk factors and generate clinical recommendations
- Identify behavioral health conditions
- Track and log services for an audit-proof record of care