Care Coordination | Patient Engagement | Care Management
SMART Goals: A Collaborative and Patient-centered Approach to Health
Comprehensive care coordination provides professional support to patients, helping them navigate healthcare and manage their health better. To that end, research on SMART goals has demonstrated its value toward patients creating healthier habits and achieving better health outcomes. When combined with motivational interviewing techniques, SMART goals establish clear, internally-motivating, and measurable goals that align with what’s most important to each individual.
Today, SMART goals are a standard part of care coordination and patient engagement.
In this article, we define this type of goal-setting, share its proven impact on health outcomes, and provide concrete tips for supporting patients to achieve success. We also review how SMART goals enable ThoroughCare’s comprehensive care coordination platform to engage, empower, and track patient progress.
The role of SMART goals in healthcare
Motivational interviewing (MI) is an evidence-based counseling style that engages patients around health issues and goals, focusing on resolving an individual’s ambivalence around making positive change. MI has been shown effective in various studies, including psychotherapy and medical plan adherence. SMART goals engage a patient’s desires and turn general health objectives into concrete, clear, and actionable targets.
Using SMART goals as part of care coordination can build rapport between the care manager or clinician and the patient. It improves communication and collaboration while demonstrating self-management skills like goal setting.
SMART goals can enhance patient morale as individuals see incremental steps and build momentum toward their intended health outcomes. And, this goal-planning approach ensures that any treatment plan is customized and balanced between what the clinician sees as necessary to improve health and aligned with patient priorities.
What are SMART goals?
The idea of “SMART” goals was first published in 1981 by George T. Doran as an acronym for rules for creating goals within business and organizational management circles. SMART stands for Specific, Measurable, Achievable, Realistic, and Time-bound.
Care managers, coordinators, or clinicians work with patients to create specific goals with well-defined criteria for success. Ensuring that goals are “SMART” entails asking questions and fettering out specific details.
SMART stands for:
Specific: Who will take what action related to this goal?
Measurable: What quantity of action will be taken? How often will this action be taken? Or what amount of action or measure of activity will be enough?
Actionable or Achievable: How will this action be carried out?
Realistic: Is this action something this individual can reasonably carry out?
Time-bound: By what deadline will this action be carried out?
Examples of SMART goals in healthcare could include:
- “John will walk outside for 15 minutes every day for the next 4 weeks.”
- “Sarah will eat no more than 1,600 calories each day for the next 2 months.”
- “Marvin will complete an ABC (Activating event, Belief, Consequence) assessment each time he feels angry for the next 7 days.”
Research demonstrates the value of SMART goals on behavior and health outcomes
Research on the effectiveness of SMART goals in healthcare and care coordination shows the value of a patient-centric, concrete approach. When implemented with adequate follow-up and support, this approach guides patients to take committed, measurable action to improve their health and well-being.
Several studies speak to the variety of use cases for SMART goals and their efficacy.
Weight loss: The U.S. Preventive Services Task Force, for example, recommends behaviorally-based methods for weight loss, including SMART goals. Analysis of 18 SMART goals studies concluded that they effectively reduced weight or improved eating behavior in 65% of studies.
Diabetes: A 2022 study published in the Journal of Pharmacy Practice found that patients who set SMART goals had clinically meaningful A1c lowering. Patients set an average of 1.5 goals during the study period and were agreeable to this technique as part of disease management. Additionally, the group using SMART goals had fewer medication changes and improved diabetes control.
Community Health: A 2021 study examined the use of SMART goals in counseling sessions conducted during community health screenings. After establishing goals with patients, follow-up revealed that 65.5% reported adherence to the SMART goal created during their initial counseling session. Patients’ goals were mainly related to diet and exercise:
- 47.4% made a diet-related goal
- 7.9% had an exercise-related goal
- 34.2% had a goal that encompassed both diet and exercise
Psychotherapy Adherence: Studies have shown that patients with behavioral health-related diagnoses can more closely adhere to their care plans and require isolation interventions less often.
While research has focused on the use and efficacy of SMART goals in various clinical and community settings, other studies highlight the need for a complementary approach to supporting a patient’s success with SMART goals.
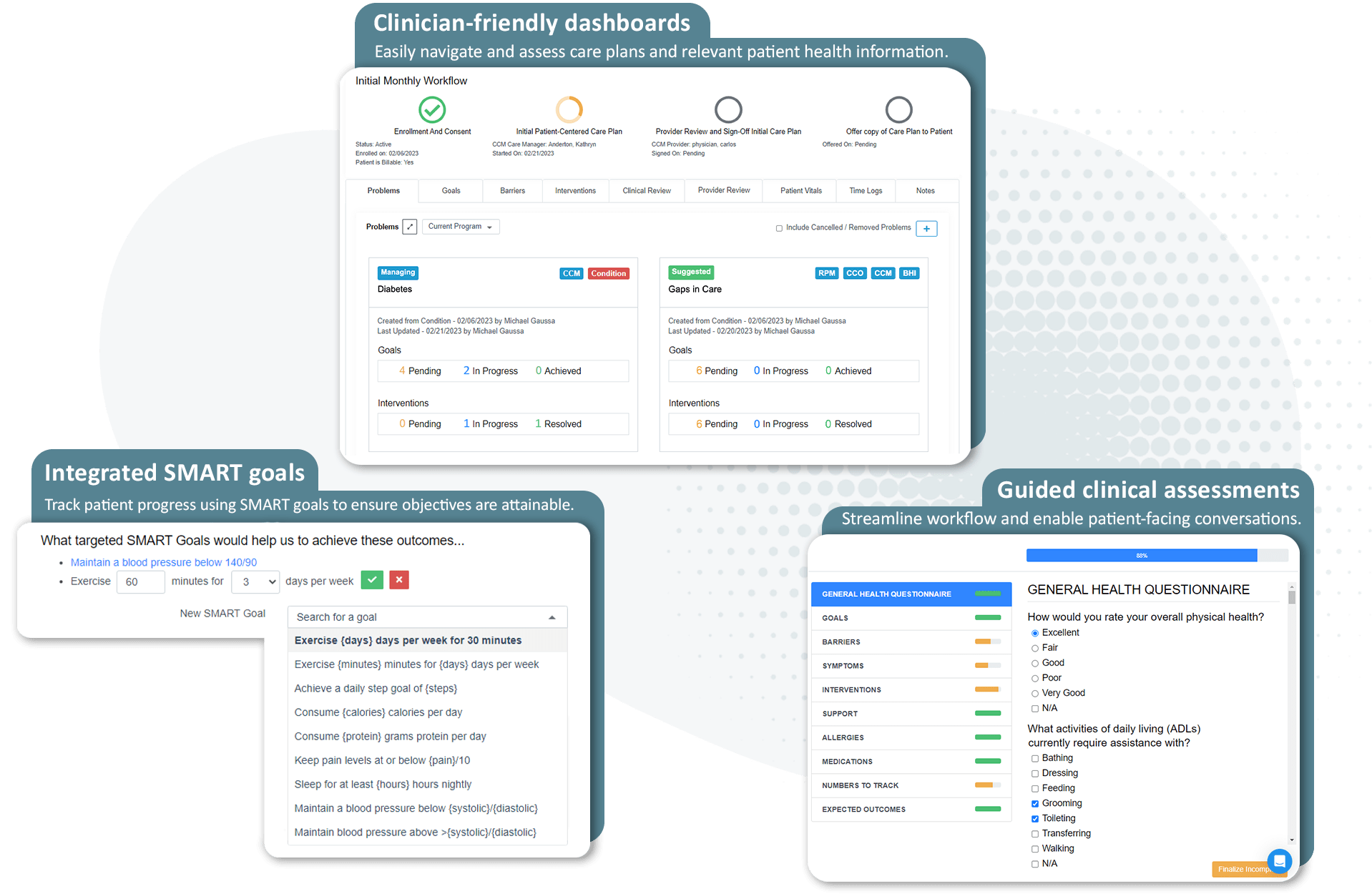
Comprehensive care: ThoroughCare helps clinicians engage patients and track SMART goal progress.
How to support patient SMART goals success
MI skills help care managers and clinicians engage patients and establish SMART goals, as well as celebrate successes and encourage ongoing progress. Additionally, the following complementary activities can further support patient goal achievement.
Moving from “what” to “how”
SMART goals focus on creating clear, concise, and patient-centered ambitions. They focus on the “what.” However, many patients struggle to envision just “how” they will carry out the tasks necessary to achieve specific and measurable goals.
Studies on SMART goals indicate the need to focus on the specific steps a patient will take and how they will deal with barriers that could derail their efforts. Care managers and clinicians who support establishing a patient’s goals can also create action plans and coping plans to help them think through a feasible step-by-step method to integrate their goals into daily life.
Also, establishing a coping plan assumes that events could thwart a patient’s efforts. Together, the patient and healthcare professional brainstorm the circumstances that might disrupt a patient’s activity toward their goal and create backup plans for what the patient will do if such a barrier arises.
Examples of coping plans could include:
- “John will walk outside for 15 minutes every day for the next 4 weeks. If the weather is bad outside, John will walk in place while watching TV for 15 minutes.”
- “Sarah will eat no more than 1,600 calories each day for the next 2 months. If she has too many snacks during the day, she will eat less at dinner and not eat after 7 pm.”
- “Marvin will complete an ABC (Activating event, Belief, Consequence) assessment each time he feels angry for the next 7 days. If he forgets or there isn’t time to complete an ABC when he feels angry, he will take time at the end of the day to reflect on the day’s events and try to complete an ABC at that time.”
A 2019 study focused on action planning for patients living with coronary heart disease. Of the 375 patients engaged by 43 physicians in eight clinical practices, 53% reported making behavior changes consistent with their action plans during a three-week follow-up. The physicians involved in the study reported that the behavior change discussion took an average of seven minutes.
Implementing SMART goals through Chronic Care Management
Chronic Care Management is a fee-for-service Medicare program. Patients with multiple chronic conditions enroll to receive ongoing care management and engagement from an assigned clinician. The program occurs on a monthly basis, over the phone or as telehealth, and creates a patient touchpoint outside of regular office visits. The clinician works with patients on:
- A monthly clinical review
- Physician reviews
- Referrals
- Prescription refills
- Chart reviews
- Scheduling appointments or services
Chronic Care Management can also leverage patient care planning to personalize interventions for specific conditions. This is where SMART goals enter the picture. Clinicians can help patients develop their care plans by establishing SMART goals and using the plan to achieve them.
For example, diabetes patients can use Chronic Care Management and SMART goal setting to account for their unique health conditions, lifestyle, and preferences. This could include identifying applicable barriers like poor diet adherence or intolerance to exercise and appropriate goals to manage.
Studies show that Chronic Care Management can reduce hospital admissions and cut health costs in the long term. Providers are also reimbursed for offering the service, helping them generate new revenue.
Tips to empower patients through SMART goals
SMART goals enable care teams to move from provider-centered instruction to patient-centered participation. Engaging in this style of goal setting leans on shared decision-making and the occasion to tap into each person’s internal motivations towards action.
“The individual’s goals should drive care coordination, but to be effective, person-centered care management also requires effective communication and coordination amongst the individual, their health care providers as well as paid and unpaid supports.” - National Committee for Quality Assurance (NCQA)
Working on establishing and achieving SMART goals offers the opportunity to build trust with patients and demonstrate respect for each person’s ability to achieve what’s meaningful to them. Keep in mind the following tips when working with a patient for the first time.
- Patients not accustomed to goal planning may need to hear the value of SMART goals in simple language. “Why should I do this?”
- While healthcare challenges may appear negative, focus on the positive and motivating reasons a patient might engage in these goals.
- Strike a balance between listening, questioning, and reflecting on what you heard. Then, turn that confirmation into a possible SMART goal for the patient’s consideration.
- Start slowly with just one or two goals to avoid overwhelming patients.
- Be sure to discuss not only the “what” but the “how” to achieve goals through clear interventions.
- Acknowledge that barriers may arise or already exist. Work together to determine what the patient will do if and when that barrier happens.
- Celebrate small wins and remind the patient of where they were when they started on this SMART goals journey.
- Ask the patient who in their life might be an encouraging or supportive goal partner and how the patient might ask for their help.
ThoroughCare helps track SMART goal progress
Providers use ThoroughCare to deliver comprehensive care management. Our platform has embedded SMART goal features that make goal setting, progress tracking, and follow-up seamless. We help:
- Streamline the creation of patient care plans
- Support staff workflows with guided, evidence-based assessments
- Help motivate patients through clinical recommendations and educational resources
- Analyze patient risk factors and identify gaps in care
- Identify and assess patients for behavioral health conditions
- Track and log services for an audit-proof record of care
- Automate CPT code assignment
Additionally, ThoroughCare supports comprehensive integration with leading EHRs, health information exchanges, remote devices, and advance care plans. Our analytics platform helps providers improve quality and performance.