Chronic Care Management | Patient Engagement
Engaging Patients is Key to Closing Gaps in Healthcare
In a previous article, we looked at foundational ways that provider organizations can close care gaps: cyclical consistency, workflow integration, and alignment with care priorities.
While closing care gaps to improve quality may seem complex, the main objective is to support patient health through the best evidence-based medicine available.
Care gap resolution isn’t about checking a box, but helping patients understand the value of prevention and health maintenance throughout every phase of life.
Yet, the vast majority of patients aren’t on board. According to a study published by Health Affairs, only 8% of U.S. adults attain all guideline-recommended services.
With that in mind, how can clinicians and their teams engage patients to gain cooperation, commitment, and energy focused on disease prevention and closing care gaps?
Preventive care challenges and the effects of care gaps
Gaps in care can result in a host of untoward effects, including:
- Patients living with certain diseases don’t know their risk level and miss timely screenings and preventative care
- Patients are diagnosed at a later stage in a disease, which can make it harder to treat, reverse, or manage it
- Patients with chronic conditions are unable to follow recommended prescription guidelines, or miss necessary testing for disease management
- Patients don’t receive recommended vaccines and boosters
- Family members, including children and grandchildren, don’t learn about hereditary risk earlier
- Comorbidities can develop that complicate existing chronic conditions
- Patients with complex clinical pictures fall through the cracks
Patients with multiple diseases or chronic conditions are particularly at risk for care gaps because of complexity, a larger and more disparate care team, and lack of coordinated care.
This leads to long-term higher costs and poor outcomes from unnecessary or repeated tests, exacerbations that lead to hospitalization, and increased patient safety and morbidity risks.
Closing gaps may require a shift in patient mindset and relationship with healthcare
It can be challenging for patients to see the big picture and grasp the prominent role that a provider plays in their long-term health. When creating and sticking to a treatment plan or complying with preventive screenings, tests, and vaccinations, patients may think, “If it isn’t broken, why fix it?”
While time and resources are precious, a provider’s success in closing care gaps requires a foundational patient understanding of how prevention and action help their health now and in the future.
They want answers to questions, such as:
- Why this…test, vaccine, medication? Patients want to know the value of investing their time, effort, and money into this activity.
- Why do I have to do this? Patients want to know why this activity is essential for them, specifically.
- Why is this important now? Patients want to know why they should make this priority today, versus years down the road.
Many patients, particularly those in a low- or rising-risk population, may not think they need preventive care because they are not sick. Additionally, patients may mistrust it, seeing prevention as a money-maker for doctors and hospitals.
Making preventive care personal
Preventive care and health maintenance should be put into the context of a person’s current and long-term goals. This is where clinicians can use personal details and motivational interviewing to highlight the importance of closing care gaps.
Put action into context: Patients brush their teeth to prevent gum disease, tooth loss, bad breath, and heart disease. Healthy habits and preventing future illness can be put into perspective similarly. Correlating daily healthy habits to taking medication or participating in screenings normalizes what some patients may view as unnecessary.
Keep what you have and help avoid future problems: Patients may need support to see that it is worth their time and effort to keep up with prevention. What patients do today will lay the foundation of their future health in three, five, or 10 years.
Healthcare’s role: Physicians and their clinical teams help patients stay healthy or become healthier by offering a schedule of preventive tests and activities that have been proven to save people’s lives.
It’s critical to build rapport and trust so that patients don’t view these activities as looking for illnesses that medicine can make money treating. Providers are screening to prevent disease or treat it earlier when it’s easier and less costly.
Conversations about risk and priorities: Patients may be aware of certain conditions that are prominent in their family, but they may not grasp the complete picture of their health risk factors, including heredity, environment, social determinants of health, and lifestyle. Risk can be multifactorial, and patients can make better choices if they more fully understand their risk profile.
Additionally, healthcare providers can connect with patient values and priorities, demonstrating that the patient and their family have much to gain or lose in the face of these risks. Relating health risks to a patient’s phase of life, potential losses from illness, and their personal goals can be an effective motivator.
The goal of preventive conversations and more extensive patient relationships is to build trust. Clinical recommendations can be more easily accepted when information is personal and easy to understand.
Establish a proactive, data-driven gap closure strategy
Whether a healthcare organization is focused on HEDIS, Star Ratings, or other care quality measures, it’s critical to create a proactive, data-driven gap closure strategy.
Research has shown that “physicians and staff spend an average of 15 hours per week closing gaps in care and satisfying quality measures, while provider organizations spend an average of $40,000 per physician per year to satisfy their quality initiatives.”
Providers and care teams that rely on specific tools and techniques can be better equipped to meet the primary driver of quality: closing gaps in care.
Population data analytics: Risk stratification and analysis of available patient data can reveal which patients or populations need timely gap closure. By proactively aggregating patient data, assessing population risk, and stratifying patients based on risk and gaps identified, providers can prioritize gaps and engage patients based on need.
Prioritize gaps based on unique patient population patterns: Prioritize preventive care discussions based on a patient’s specific clinical risk factors, as well as the likelihood that a particular preventive screening will impact the patient’s quality of life. And, because specific preventive measures can have a greater impact than others, clinicians may be able to focus on fewer high-value gaps during encounters.
Implement quality scorecards: Timely and actionable quality scorecards are a tool to help focus the care team’s attention on relevant care gaps. Figure 1 shows an example of a scorecard for two care standards—breast cancer and colorectal cancer screenings.
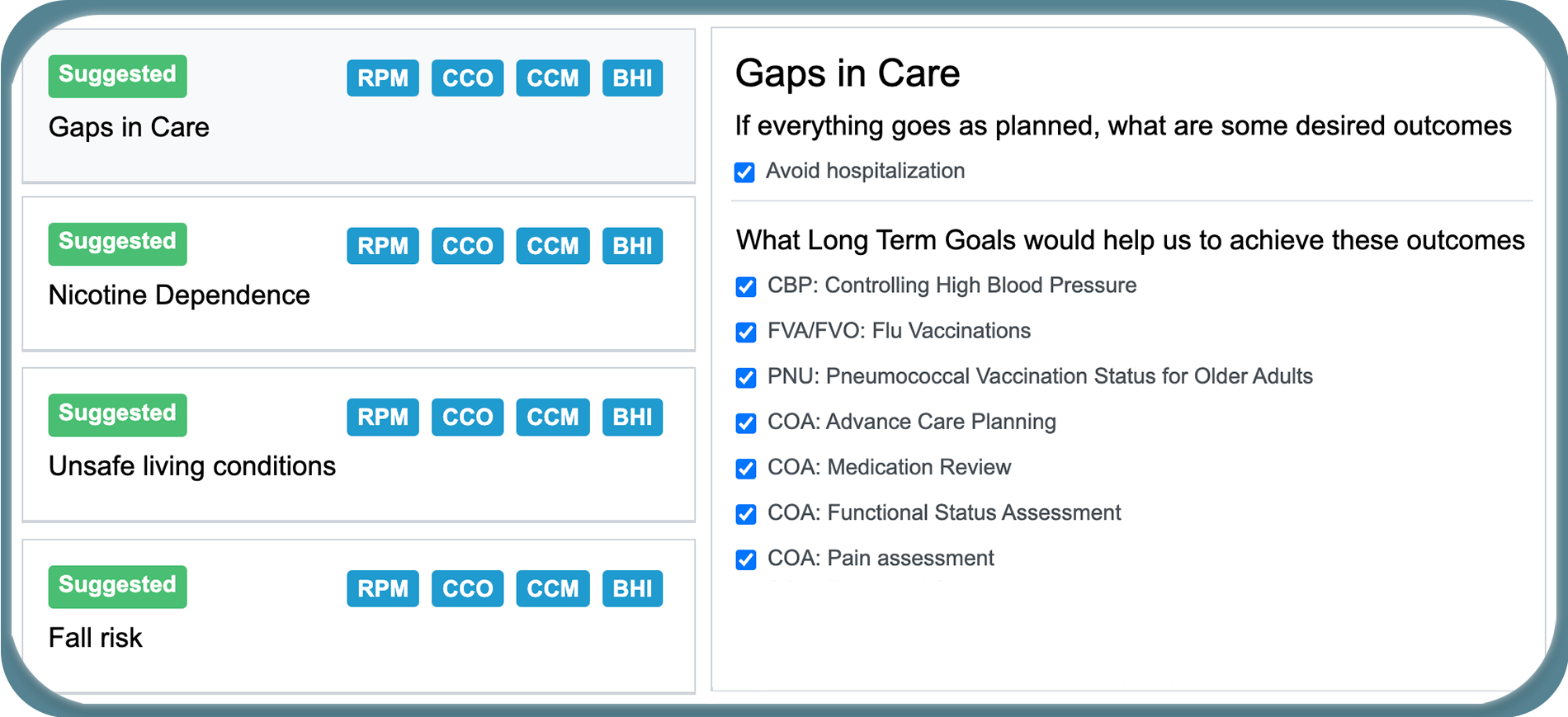
ThoroughCare enables clinicians to close suggested gaps in care.
Emphasize Annual Wellness Visits: Claims data can be a straightforward way to identify patients who have not been seen before the measurement period ends, but it can be challenging for providers to access.
However, care teams can prioritize Annual Wellness Visits by creating patient lists in early September. They can then launch a campaign to see patients before the end of the measurement year.
Create a Health Maintenance Month: Related to AWVs, consider establishing a health maintenance month where patients are contacted ahead of time to promote the importance of preventive and health maintenance tasks. Similar to maintaining cars, homes, and other things patients value, a health maintenance month highlights the need to invest time and energy in health.
Leverage a Chronic Care Management Program (CCM): Coordination is invaluable in closing HEDIS and other types of care gaps. Chronic Care Management programs are uniquely positioned to use consistent communication and connection to address care gaps.
Establish a communication strategy and process: Provider organizations may wish to create a policy or instructions for communicating with patients, particularly about care gaps preventive and health management topics. Determine how staff will capture the patient’s preferred and most trusted type of communication—text, email, in-person, or phone—and how this will be practically implemented through software and operational procedures.
Closing care gaps takes time, energy, and planning. However, what’s most important is engaging patients with methods that ensure individuals understand the value of these activities.
How ThoroughCare can help
Approximately 700 care delivery organizations use ThoroughCare to manage and coordinate care, as well as close care gaps. With seamless EHR integration and data interoperability across health information exchanges and remote devices, our platform supports solutions for:
- Chronic disease management
- Remote patient monitoring
- Behavioral health services
- Wellness assessments
- Transitional care
Providers use ThoroughCare to seamlessly manage patient populations, create and maintain patient-centered care plans, motivate and engage, and visualize and interpret data to inform care decisions.



