Chronic Care Management | Social Determinants of Health
Understanding Social Need, Social Risk, and Social Determinants of Health
Health plans and provider organizations are beginning to wrestle with the non-medical influences that significantly affect patient health.
Referred to as social determinants of health (SDOH), they include factors like socioeconomic status, education, neighborhood and physical environment, employment, social supports, and access to healthcare.
Assessing these factors can indicate the level of social risk and social need that create barriers for patients to receive timely, adequate care and achieve better health.
However, for healthcare leaders who want to support clinical and non-clinical aspects of wellness, identifying the subtle differences among these concepts is critical. This understanding can help create meaningful change.
Social drivers, social risk, and social needs are interrelated but distinct
These three concepts are often used interchangeably. Yet, their definitions highlight essential differences.
- The World Health Organization defines SDOH as "the conditions in which people are born, grow, live, work, and age." They are shaped by the distribution of money, power, and resources. They are the broad policies, laws, and systems that affect large populations.
- Social risk factors are specific adverse social conditions associated with poor health. They include issues like social isolation and housing instability, which directly affect health. They may affect some sub-populations and regions more than others.
- Social needs refers to "health-related social needs." These include the social and economic conditions individuals experience that affect their ability to maintain their health and well-being. They reflect access to care, personal resources, and capacity to make healthy choices.
The image below puts these concepts into context.
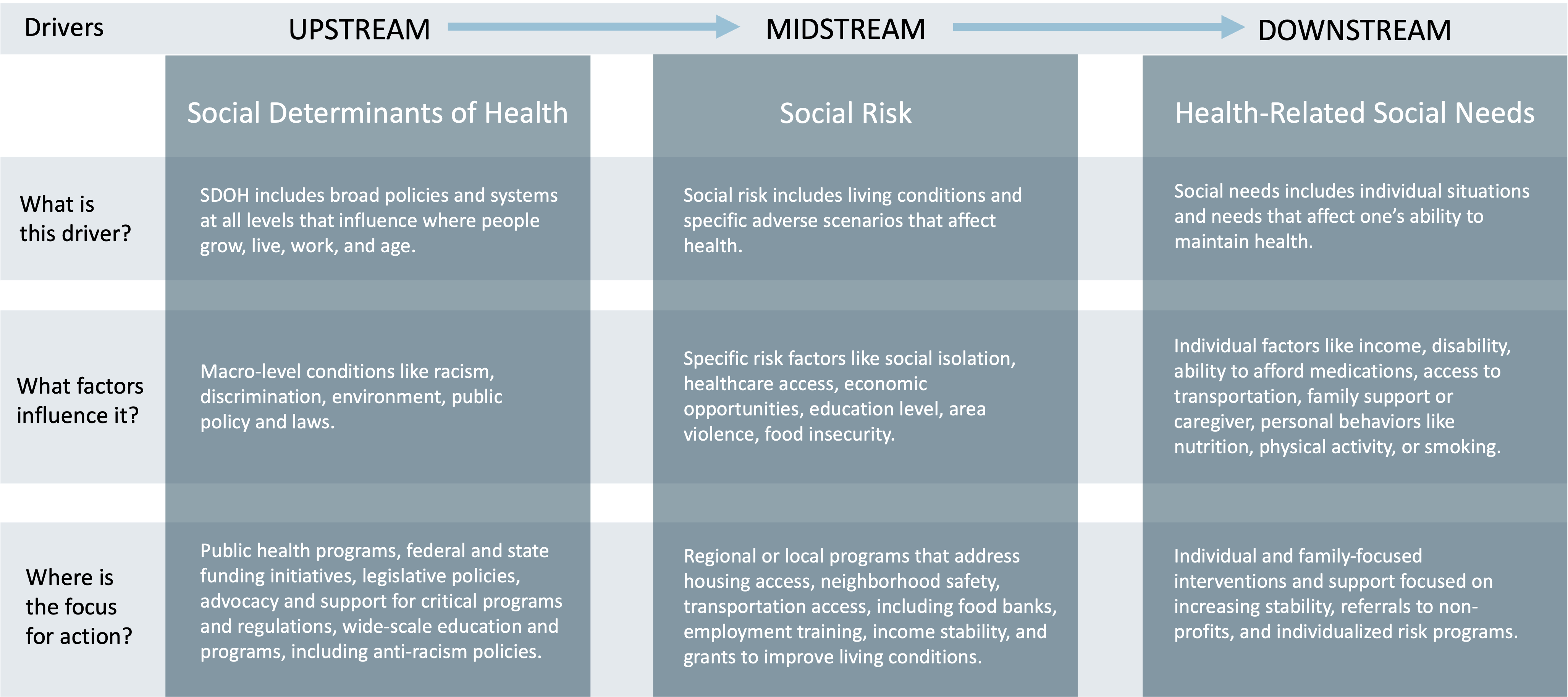
From this perspective, it’s easy to see how various factors create negative impacts, moving from populations to individuals. This vantage point can also serve as a map that healthcare leaders can use to focus on which issues and programs could best fit their capabilities.
Where are healthcare organizations investing in social determinant-related efforts?
Most healthcare organizations focus on individual social needs and social risks.
Consider that from 2017 to 2019, hospitals alone spent $2.5 billion on social determinant programs. In that time, 57 health systems, including more than 900 hospitals, developed 78 unique programs involving social determinants.
These organizations focused mainly on downstream and midstream interventions, including:
- Housing ($1.6 billion)
- Employment ($1.1 billion)
- Education ($476 million)
- Food security ($294 million)
- Social and community context ($253 million)
- Transportation ($32 million)
During the COVID-19 pandemic, social needs increased dramatically, which was confirmed by research by KFF:
- 13.6% of adults reported that they, or someone in their household, recently experienced a loss of employment income
- 61.3% reported difficulty paying for usual household expenses the previous week
- 31.8% used credit cards or loans to meet household spending needs
- 7% of adults expressed no confidence in their ability to pay the next month’s housing payment (across renters and owners)
- 10.3% reported food insufficiency in their household
- 31.4% reported symptoms of depression or anxiety
In response, the 20 largest health plans increased investment into SDOH by more than 1.6%, spending more than $1.87 billion over a five-year period. Their main focus was on housing ($1.2 billion) and food security ($238 million), with smaller investments into employment, education, transportation, and community support.
SDOH initiatives focus mainly on midstream and downstream issues
Investments like those made by health systems, hospitals, and payors tend to focus on social risks and needs rather than upstream drivers.
While some leading healthcare organizations advocate for broader change at the regional, state, and federal levels, most look to uncover issues that negatively affect the health of their local community and residents.
Through community partnerships, value-based care agreements, and direct investment, organizations can embed social risk and social need assessments into existing accountable care or advanced primary care programs and care management services.
Upstream initiatives tend to include:
- Assessing an organization’s cultural sensitivity
- Carrying out health equity assessments
- Creating health equity-focused policies
- Engaging in broader public policy work or advocacy to support anti-discrimination and inequities larger populations face
Incorporating social risk and social needs into existing care delivery
There are many ways that healthcare organizations may begin to identify and address various SDOH factors that may create barriers to patient health.
Community health assessments
Conducting a health equity-focused community assessment can be a first step. It can help identify patient populations that need the most support and uncover their most significant barriers.
Armed with regional assessment information, healthcare leaders can use data science to analyze how these issues affect specific patient populations.
Social risk scores
Area-level indices and social risk scores, like the Area Deprivation Index, Social Vulnerability Index, or Neighborhood Deprivation Index, can help connect local issues to identified patients.
Health-related social needs screening
Adopting standardized social risk screening tools will enable care teams to gather critical patient data, as well as uncover specific needs. The Institute of Medicine previously established 11 SDOH data domains, focusing on violence, education, financial strain, race/ethnicity, social support, and neighborhood income.
The Centers for Medicare & Medicaid Services (CMS) has recommended prioritizing domains that can be addressed through community services, including:
- Housing instability
- Food insecurity
- Transportation access
- Utility assistance
- Interpersonal safety
Several screening tools offer a standardized and vetted way to capture patients’ social needs.
For example, the Protocol for Responding to and Assessing Patients’ Assets, Risks, and Experiences (PRAPARE) is a nationally standardized patient risk assessment protocol. Its validated assessment tool has been translated into 25 languages and is based on a set of national core measures.
PRAPARE is evidence-based and able to be used in conjunction with ICD-10, LOINC, and SNOMED.
The Health-Related Social Needs Screening Tool was developed by the Center for Medicare and Medicaid Innovation. It includes 10 items categorized into five domains and can be patient-administered or used by professionals.
The American Academy of Family Physicians also created an 11-question SDOH short form in English and Spanish that can be self-administered or delivered by clinical or non-clinical staff.
Maximizing positive impact on health through SDOH programs
Payors, providers, and healthcare advocates are working beyond direct clinical areas to support patients who face societal and economic barriers to better health.
With a greater understanding of the vital differences among social drivers, social risk, and social needs, healthcare leaders can bring clarity and garner internal and external support for making investments that align with the organizational mission.
How ThoroughCare can help
ThoroughCare can help payors and providers deliver digital care coordination. Our platform helps care teams engage patients and address barriers to chronic care management.
Our solution can:
- Streamline the creation of patient care plans
- Support staff workflows with guided, validated assessments
- Help motivate patients through clinical recommendations and SMART goals
- Analyze patient risk factors and generate clinical recommendations
- Identify behavioral health conditions
- Monitor key performance metrics to spot gaps in care
- Track and log services for an audit-proof record of care
Additionally, ThoroughCare supports comprehensive integration with leading EHRs, health information exchanges, remote devices, and advance care plans, while helping providers visualize and interpret operational data through analytics.



