Chronic Care Management | Patient Engagement
Engaging Patients with SMART Goals for Chronic Care
Engaging patients has become more of a focal point for healthcare. Motivated people tend to believe in their ability to improve or maintain their quality of life.
“The objective is not to solve the patient's problem or even to develop a plan; the goal is to help the patient resolve his or her ambivalence, develop some momentum, and believe that behavior change is possible,” according to the American Academy of Family Physicians.
Could patient motivation tools and techniques help reduce costs and improve care quality?
Value-based care has asked payors and providers to adopt an enhanced, patient-centered approach to care coordination and chronic care management. SMART goals, for instance, further this approach by inviting patients to collaboratively set their own benchmarks.
Shift from disease-centricity to person-centricity
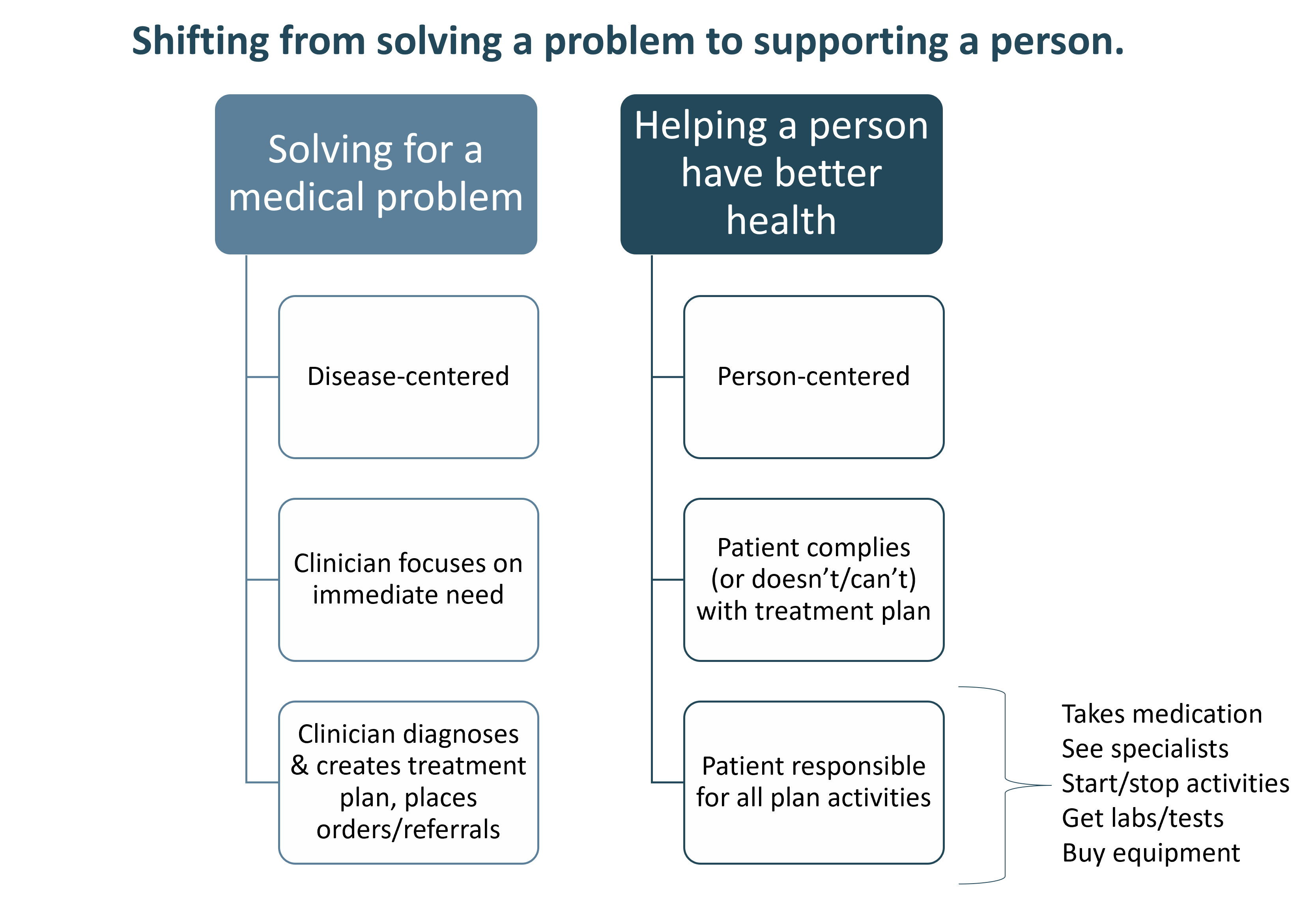
Medicine has traditionally been a disease-focused, unidirectional paradigm, as reflected in the graphic below.
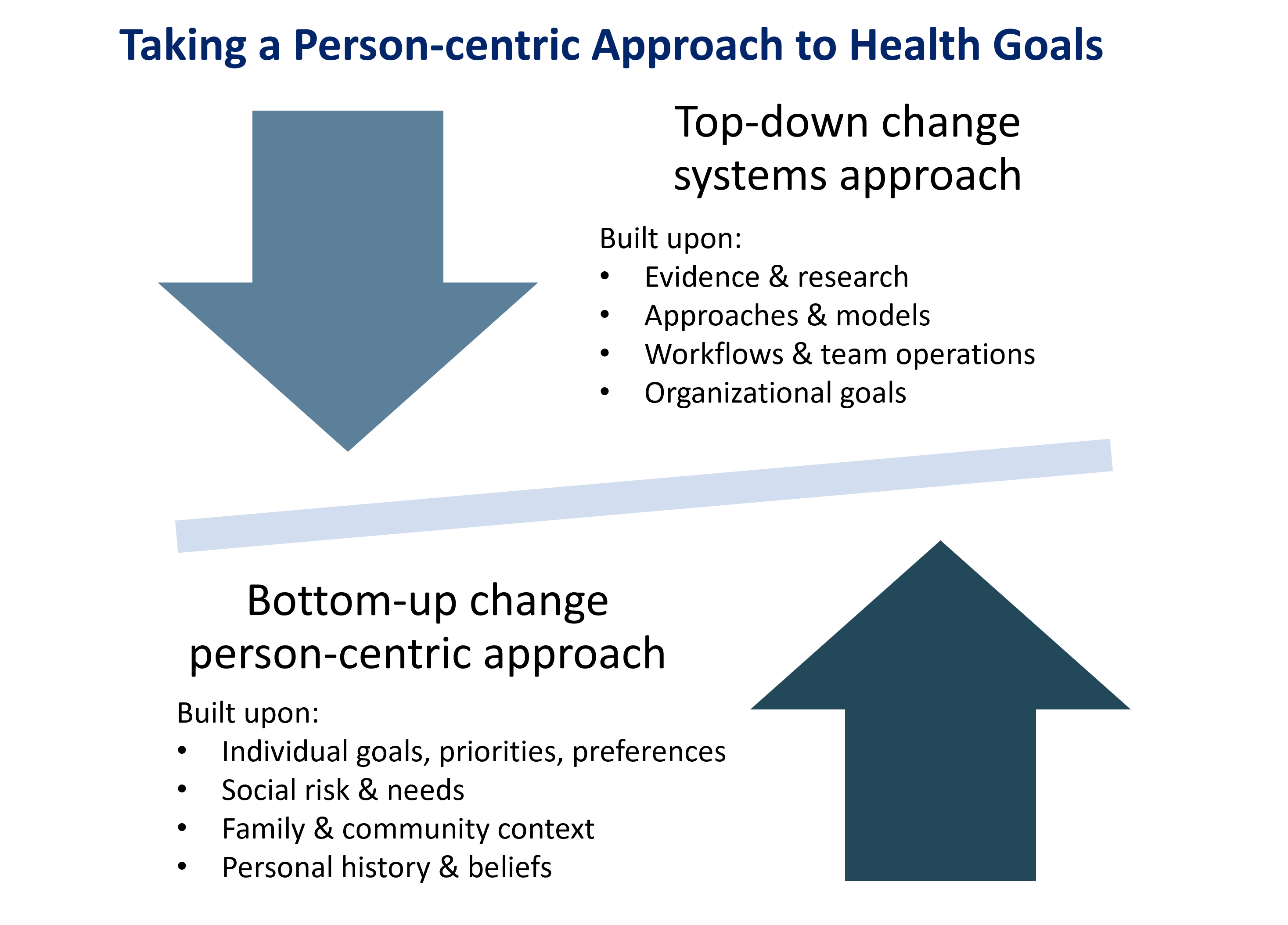
The physician assesses the patient and provides a diagnosis and treatment plan. The patient takes the treatment plan and is expected to implement it as given.
However, this top-down approach fails to achieve the modern aims of high-quality, cost-efficient, and outcomes-oriented healthcare.
Chronic disease needs a personalized approach
A linear approach to chronic disease management falls short. It can fail to provide the type of comprehensive, supportive environment and solutions to help realize life and health goals.
“Outcomes should cover the full cycle of care for the condition, and track the patient’s health status after care is completed,” according to Harvard Business Review.
But how can clinicians and care teams provide a more person-centric approach that ensures overall success?
Person-centered care through a goal-oriented approach
Goal-oriented care engages patients in identifying their personal objectives and aligning their care with these desired outcomes. While providers may have population- or performance-metrics to achieve with their patients, that objective must be balanced with what the patient deems of primary importance.
According to researchers in PLoS One, “The focus on setting goals based on the patient’s needs and preferences rather than on health-related outcomes became one of the main novelties in chronic disease management.” The same could be said of chronic care management.
As an evidence-based medicine (EBM) model, goal-oriented care taps into tools like SMART Goals to strike a balance between the best available practices, the provider’s clinical expertise, and the patient’s values and preferences.
As a standard part of care coordination and patient engagement, SMART Goals engage a patient’s desires and turn general health objectives into person-driven targets that are concrete, clear, and actionable.
But, before approaching the subject of tactical goal setting, it’s important to ponder and appreciate the patient’s perspective.
Embody the patient’s perspective
Providers are called to care for an evolving population of patients: a more diverse group living longer with more chronic illnesses and varied experiences and needs.
Having a broader view of how and why a patient thinks, acts, and decides can maximize the value of every patient-provider relationship, as well as their positive impact.
A study published in the Annals of Medicine found that better patient-provider relationships can mean better patient outcomes. Patient-provider relationships were positively associated with functional health status by a correlation coefficient of 0.2.
The article spoke to this association, stating, “When patient-provider relationships improved, functional health status also improved by a correlation coefficient of between 0.05 and 0.08. Conversely, when patient-provider relationships deteriorated, as did functional health status.”
Here are four ways to think differently from the patient's perspective.
These could improve patient satisfaction by impacting the four core elements of the provider-patient relationship, including trust, knowledge, regard, and loyalty.
Know me: What’s meaningful and most important
Making long-term health behavior changes is difficult for the most disciplined patients. It’s why estimates put the percentage of people consuming a healthy diet at 37.9% and those achieving the recommended amount of physical activity at 46.5%.
Helping patients improve their health and well-being can be most effective when it taps into their desires, preferences, and motivations.
Numerous studies have shown that intention to change behavior alone does not consistently result in behavior change. Providers and care management teams can support patients to overcome the intention-behavior gap by tapping into an individual’s goals and priorities.
Programs like chronic care management and behavioral health integration can equip patients to take action.
Help me: Make the connection and overcome barriers
A lack of health literacy can prevent people from making well-informed choices. When a patient has information, they often can improve behaviors. However, it seems that just knowing isn’t enough to overcome long-standing beliefs and assumptions.
Some patients may hear erroneous information from family or the media. They may have had poor or discriminatory healthcare experiences and don’t trust medical professionals. Or cultural norms may negate sound medical advice.
Here, taking time to fetter out the assumptions without judgment is essential. Making the connection between a patient’s disease and its accurate cause can be challenging but effective in understanding a treatment plan.
Trust and understanding are powerful in a patient-clinician partnership.
Respect me: Being transparent with provider goals
In goal-oriented, patient-centered care, the provider is an advisor and facilitator rather than a medical expert or technician. At the physician’s direction, a care manager provides ongoing support to help patients set and achieve their goals.
However, it’s vital that a provider helps the patient understand their pressures and underlying objectives as the patient’s healthcare partner. Providers are charged with meeting various population, quality, and care goals, but patients are unaware of this fact.
Collaborating as partners means that providers listen and respect patients and provide transparency to the larger environment that drives their decisions and recommendations.
Connect with me: Clear, compassionate, and culturally sensitive communication
With little time for patient appointments, providers can struggle to take time for active listening and open-ended questioning.
However, putting aside personal preferences and acknowledging one’s tendency toward bias can create a more trusting and open environment that could lead to better alignment on care goals.
When the care team is trained in cultural humility and motivational interviewing, goal-oriented care can lead to mutual decision-making and cooperative care plan implementation. Providing clear, compassionate, and sensitive communication builds a patient’s confidence and empowers them to work collaboratively in establishing and accomplishing SMART goals.
Amplify SMART Goals from the patient’s perspective
Providers and care teams can create more fruitful patient relationships when they’re built through open communication. This approach can generate understanding and motivation while respecting the patient’s goals and priorities.
How ThoroughCare Can Help
ThoroughCare’s intuitive software platform can help providers collaborate and deliver digital care coordination and chronic care management. Our solution can help:
- Streamline the creation of patient care plans
- Support staff workflows with guided, validated assessments
- Help motivate patients through clinical recommendations and SMART goals
- Analyze patient risk factors and generate clinical recommendations
- Identify behavioral health conditions
- Monitor key performance metrics to spot gaps in care
- Track and log services for an audit-proof record of care
Additionally, ThoroughCare supports comprehensive integration with leading EHRs, health information exchanges, remote devices, and advance care plans, while helping providers visualize and interpret patient and operational data through analytics.



