Principal Care Management | CPT codes
2023 Principal Care Management CPT Codes: 99424, 99425, 99426
Understanding the CPT billing codes for Principal Care Management (PCM) will provide you with a better idea of what is expected, both by the patient and by Medicare.
Understanding billing codes can also help you project revenues and optimize your staff’s capacity.
At ThoroughCare, we’ve worked with clinics and physician practices nationwide to help them streamline and capture Medicare reimbursements. Our software solution assists with the rules and regulations for PCM while also tracking all activities related to providing the program and easing the difficulties of billing.
What is Principal Care Management?
PCM is similar to Chronic Care Management (CCM) in the treatment of chronic conditions, but PCM is refined in scope to the treatment of an isolated chronic condition.
PCM was designed by the Centers for Medicare & Medicaid Services (CMS) in 2020 to provide care services that concentrate on treating one chronic diagnosed illness. This program also pertains to patients with more than one chronic diagnosis if the provider focuses solely on one, single individual chronic condition.
Patient qualifications for PCM include:
- A diagnosis is expected to last between, at minimum, three months to life-long
- The condition being treated must place the patient at significant risk of death, acute exacerbation or decompensation, or in a state of functional decline, and/or be associated with a recent hospitalization
- Written or verbal patient consent documented by your practice
PCM services are delivered through remote interactions, easing the burden of patient travel to your practice. These services can include:
- A monthly clinical review
- Telephone calls
- Physician reviews
- Referrals
- Prescription refills
- Chart reviews
- Scheduling appointments/services
Services rendered are driven by the patient’s individual care plan, which is created in collaboration with the patient upon PCM enrollment. Care plans serve as a comprehensive guide to a patient’s goals, health history, and behavior.
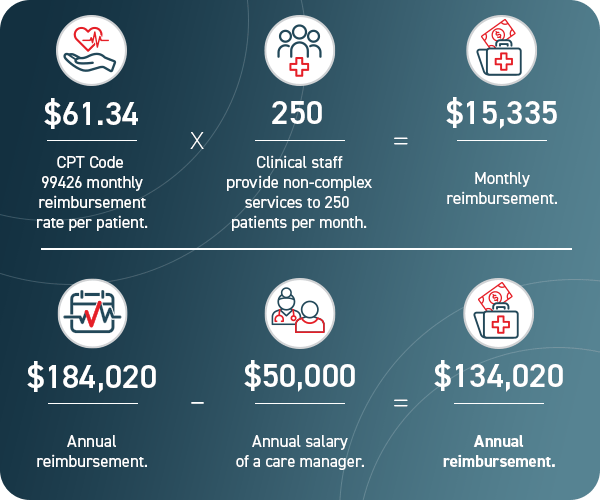
Medicare Part B covers 80% of this benefit for patients. Practices, on average, can receive $61.34 for 30 minutes of clinician-service time per month. Additional opportunities to meet higher billing thresholds are also available.
PCM can strengthen the relationship between your patients and your practice. The program’s structure, with monthly touchpoints and care team access, can improve patient engagement.
How to Bill for Principal Care Management
Unlike CCM with a 20-minute requirement for billing, PCM has a 30-minute requirement for billing reimbursement. It is an important distinction.
Five items are required when submitting a claim through CMS:
- CPT codes for each program you are managing for the patient
- ICD-10 codes tied to each of the conditions you are managing within that program
- Date of service
- Place of service
- National Provider Identifier (NPI) number
It is not necessary to know the care manager assigned to the patient, but it is helpful in case of an audit. When billing, calculate the time spent with each of your patients monthly.
Four steps are required to bill for PCM:
- Verify CMS requirements were met for each patient each month
- Submit claims to CMS monthly
- Send an invoice to patients receiving PCM services monthly
- Make sure there are no conflicting codes that have been billed
CPT Codes for Principal Care Management
See 2025 reimbursement rates here.
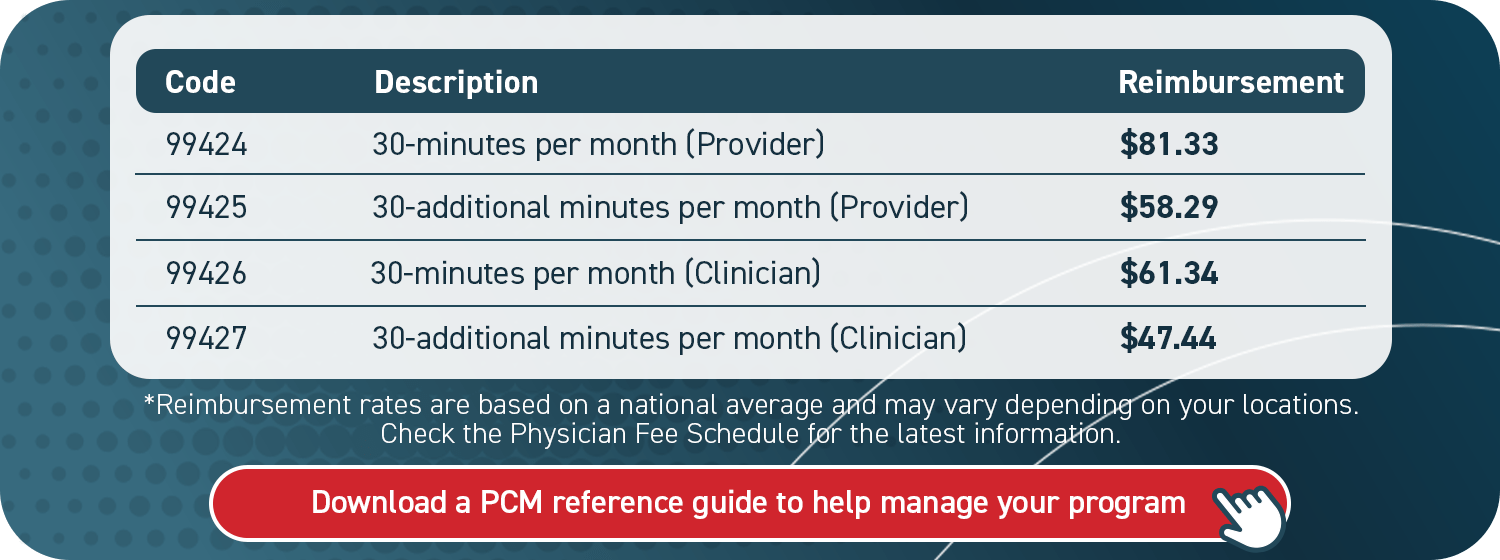
As indicated by the following chart, there are four types of PCM billing codes available.
As shown, one set of codes (99424 and 99425) is designated for providers’ utilization in 30 and 60-minute increments. The other set of codes (99426 and 99427) is for clinical staff usage also in 30 and 60-minute increments of service.
Although there may not be any difference in the services delivered between the provider and clinician code, it is important to note that utilizing the most appropriate code for who delivered the services is considered best practice in case of an audit by Medicare.
The determination between utilizing provider or clinician CPT codes would hinge on patient case complexity and provider discretion.
It is important to note that a provider cannot offer both CCM and PCM services to the same patient in a given month. However, the patient may receive PCM services from one provider and CCM services from another provider as long as the different conditions are being managed in both of the programs.
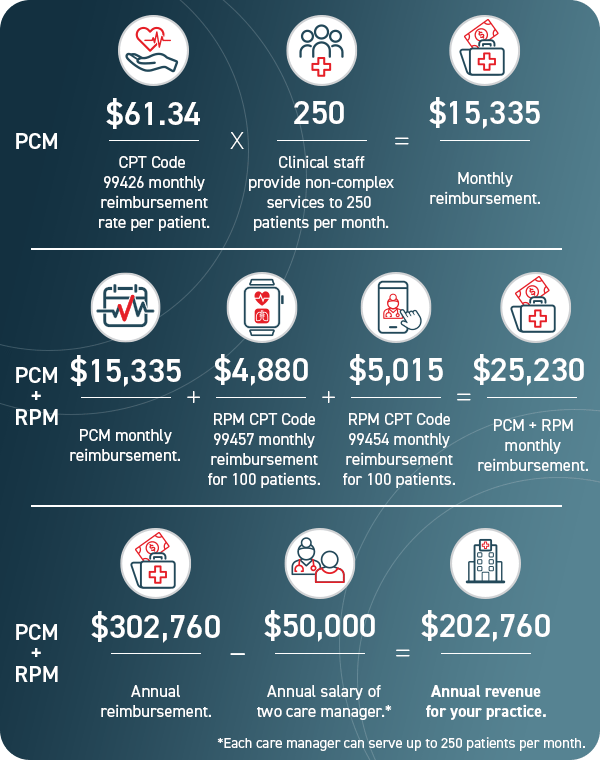
Principal Care Management in Conjunction with Remote Patient Monitoring
Medicare allows patients to enroll simultaneously in both PCM and Remote Patient Monitoring (RPM). Together, the two programs can inform a more holistic approach to chronic disease management.
RPM enables clinicians to track patients’ vital signs through the transmission of data via digital devices. It is often used to monitor chronic conditions by collecting this information daily. While working within the PCM program, RPM data can inform care decisions employed to manage a chronic condition.
For instance, your practice can use RPM to measure and trend blood pressure and blood glucose levels that influence a patient’s condition, monitoring these over time. These two programs are inherently compatible.
Patient consent is required for both programs. In the event of a Medicare audit, patient consent documentation is required. Care coordination software can automatically document the required patient consent.
When billing for both PCM and RPM, record billable time for each individual program. For instance, PCM is billed in 30-minute increments and RPM in 20-minute increments; utilize the applicable CPT codes for all services rendered across both of these programs.
How Principal Care Management Produces Revenue
Revenue opportunities are available for your practice within PCM.
Your practice’s revenue can increase dramatically by utilizing RPM in association with PCM.
An undeniably valuable aspect of the PCM program is not simply the potential revenue, but also the broader reach of care access for patients. It stands to reason that easier care accessibility could also increase patient numbers and, therefore, revenue.
Streamline Principal Care Management with Care Coordination Software
Knowing the CPT codes for PCM can help your practice project revenue and optimize your care team’s capacity. But to deliver and document PCM services utilizing best practices, a system needs to be in place to manage your program.
A practical resource, such as care coordination software, secures key details from being lost or overlooked. This promotes efficiency for you and your staff, which subsequently helps patients to succeed. Care coordination software can streamline the creation of patient care plans, support staff workflows, and simplify billing.
ThoroughCare’s software solution offers these exact features.
With a clinician’s eye, we’ve designed an intuitive platform that untangles the PCM process, so both you and your patients can benefit. Our care coordination software enables you to offer a whole suite of wellness services that pair well with PCM, such as RPM and Transitional Care Management (TCM).
Reimbursement rates are based on a national average and may vary depending on your location. Check the Physician Fee Schedule for the latest information.