Care Coordination | Value-Based Care
Value-based Care Solutions: Team-based Care Coordination
Several factors are driving the adoption of team-based care coordination. Workforce shortages exacerbated by the pandemic, a growing population of adults living longer with chronic disease, and the shift toward value-based care models top the list.
The Institute of Medicine (IOM) defines team-based care as being delivered by at least two healthcare providers. This includes coordinated collaboration with patients and their caregivers to accomplish shared goals within and across settings.
The Agency for Healthcare Research and Quality (AHRQ) defines care coordination as “deliberately organizing patient care activities and sharing information among all of the participants concerned with a patient's care to achieve safer and more effective care.”
When combined, team-based care coordination can help providers and payors support streamlined, more efficient service delivery. This can lead to consistent patient engagement and help achieve better outcomes in health and cost.
What’s driving team-based care adoption?
Healthcare is more focused on diagnosing and treating chronic conditions than in the past. As people live longer with more chronic illnesses, healthcare resources and costs have shifted. Additionally, chronic condition management requires various support types over more extended periods. Physicians alone can’t keep up with the volume, nor is it the most efficient use of their training.
Even when medical practices employ additional professionals, such as nurse practitioners and physician assistants, staff shortages still make an impact. This is leading providers to divide and assign patient care tasks into finer categories, including the level of license, skills, and training required.
Value-based care programs leverage this approach to maximize the value of each team member and control overall costs.
Plus, in today’s digitally connected healthcare environment, more is being asked of clinical and administrative staff. For example, the volume of patient portal messages has risen dramatically since the pandemic. One EHR vendor reported a 157% increase in incoming patient messages during the pandemic's first year, with each message requiring physicians to spend an average of 2.32 additional minutes in the EHR.
Team-based care provides one of the best strategies to maximize patient impact, streamline complicated care, and share the workload. This can make the best use of each member’s skill set and formal training.
Benefits of team-based care
Research has demonstrated that team-based care can improve utilization, decrease healthcare costs and improve health outcomes. Studies have highlighted just some of the benefits of team-based care and care coordination, including:
- Reduce adverse events like hospital readmissions and duplicative testing
- Streamline care fragmentation
- Expand access to care through more coverage and shorter wait times
- Increase job satisfaction and improve experience measures reported by patients, staff and physicians
One study found that adults experienced higher quality and lower acute care utilization.
Other research has shown that non-physician professionals can be effective in helping patients achieve better health. For example, among 19 studies comprising 5,993 participants, non-physicians were able to help patients achieve twice the decrease in 12-month systolic blood pressure versus titration via a physician.
When teams are supplemented with care support professionals, such as social workers, pharmacists, and care coordinators, team-based models can successfully implement more comprehensive or value-based services for complex and rising-risk patients.
Characteristics of successful team-based care models
Care coordination for chronic disease management is generally built on team-based care, communication, and data via technology tools. Within that discipline, team-based care relies on five principles, according to a discussion paper published by the IOM and authored by Mitchell et al., including:
Shared goals – The team, including the patient and appropriate family members, collaborate on priorities that reflect the patient’s desires in conjunction with good medical practice.
Clear roles – Each team member understands their function, responsibilities and accountabilities. When roles are delineated and documented, the collective team creates a synergy that results in greater efficiency, leading to less friction and waste.
Mutual trust – The team creates strong working norms of support, education, respect and shared achievement that build trust and reliability.
Effective communication – There is a commitment to candid, complete communication that is reflected on and refined over time.
Measurable processes and outcomes – The team is guided by specific quality and performance targets. The team incorporates learning and improves quality iteratively through regular review and feedback.
Team-based care operational best practices
In addition to committing to the previous principles, care teams focused on chronic care management or value-based care models should consider incorporating several best practices to maximize their impact. These include:
Team huddles – Daily huddles can take 5-15 minutes to bring intention, focus and clarity to the day ahead. It’s also an opportune time to reiterate procedures or new processes. A standard agenda gives structure and efficiency. Huddles also enable the team to highlight possible challenges for the day and patients who may need additional support.
Medicare Annual Wellness Visits (AWV) – These proactive reviews provide an opportunity to close care gaps, build rapport with the patient, and set future preventive health goals. AWVs can be performed by independent clinicians, such as physician assistants, nurse practitioners and clinical nurse specialists, or other licensed medical professionals. These include health educators, registered dietitians or nutritionists under physician supervision.
For chronic care management, or other team-based care models, the AWV becomes the foundation of managing chronic disease, engaging patients regularly and preventing future illness.
Panel management reviews – This kind of team huddle focuses on reviewing and developing action plans for individual patients. Held regularly, panel reviews can hone in on a specific population health group, such as patients with frequent emergency room visits, high social risk scores or frequent readmissions.
While the team should already be aware of these patients, panel management provides time to look at patterns in the population. This review can help strategize ways to improve health, utilize available resources, or implement short-term campaigns to engage patients.
Annual prescription renewal – Where appropriate, physicians and their teams renew all chronic medication prescriptions for chronic care management patients once a year. This provides 15 months of medication authorization of a 90-day supply and four refills.
This can help improve medication adherence and save the team valuable time. And, if the patient’s medication for a chronic condition changes, a new prescription can replace the previous one.
Review physician tasks list – There are many individual tasks that physicians can delegate. A comprehensive review of general responsibilities reveals potential areas that could be delegated and to which team member(s). This review should also discuss what changes need to be made to operating procedures, workflow and technology access or setup.
A sampling of the types of physician tasks that could be delegated include:
- Performing traditional rooming duties (intake, allergies, medications, vitals, etc.)
- Determining chief complaint
- Taking a preliminary history of present illness/review of systems
- Administering pre-ordered vaccines
- Implementing plan (pending orders)
- Updating problem lists
- Providing educational resources
- Completing forms, letters, etc.
- Scheduling follow-up visits
Taking a proactive approach to team-based care design
Creating a strategic and thoughtful team design is paramount, especially for participation in the ACO Investment Program or Making Care Primary.
Here are three approaches to help ensure team construction meets care delivery, financial goals and constraints.
Inventory existing and needed skills and capabilities
Start by creating an inventory of existing workflow and team abilities that align to different professional licenses or roles.
Below is an example of a task grid where existing team activities and their corresponding licensures are captured. At this point, the goal is to note current task categories and who performs them.
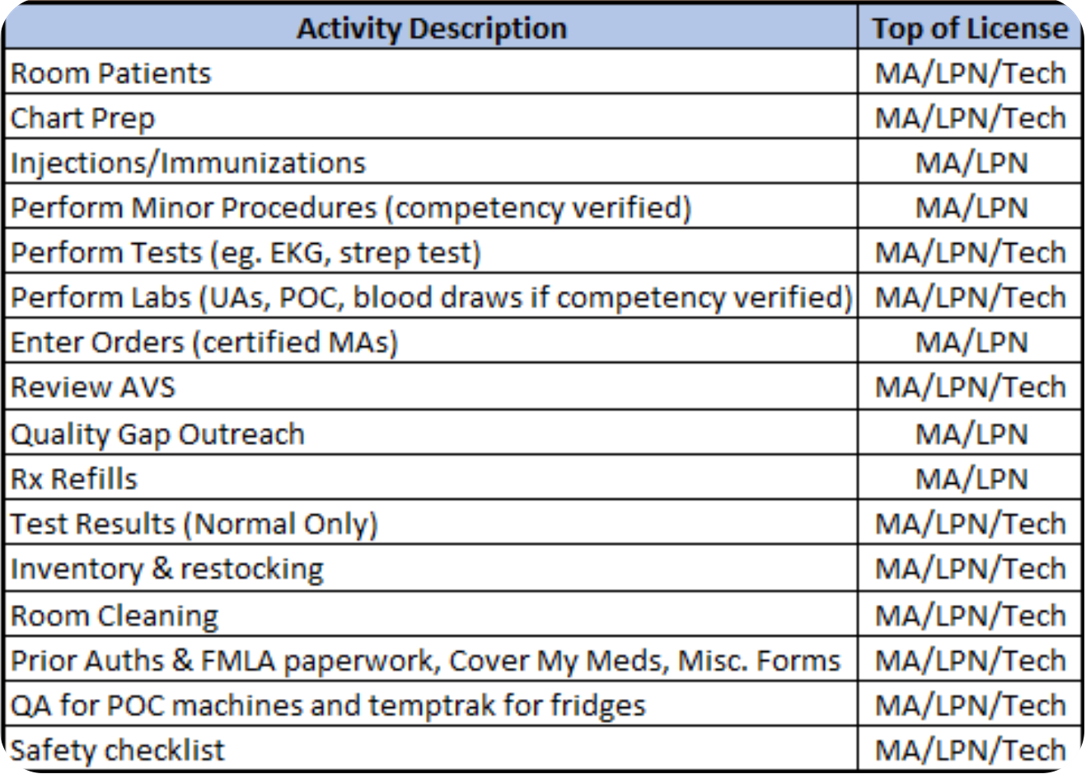
Figure 1: Closing the Gap: Team-Based Care Models. Presentation by Rackmil and Sego, nursing executives, for Sigma Theta Tau International, 2022.
Then, make note of the capabilities, skills and licenses needed for the new team-based model. Value-based care specifies the types of activities required, which can be mapped to roles.
For chronic care management teams, billing and reimbursement rules provide a starting structure.
Assess licensure opportunities for expanded roles
Note these needed functions as they represent gaps in the existing team. They represent ways to expand staff responsibilities or highlight hiring priorities.
This is a critical step because it clarifies opportunities for existing staff growth or where a budget could enable hiring. New roles could deliver expanded capabilities for the provider.
Map team design to current or possible operational structure
Workflow mapping can occur once the ultimate team design is complete.
From a strategic viewpoint, think about how transitioning from the current to the new team —or creating a new team—may impact the provider organization.
What new services does this team enable? How would operations and procedures need to evolve? What would this new structure mean to leadership and management?
It’s important to note that the team design should be independent of the individuals who may hold those positions now. Focus on what the function or role should entail. Then, note how the individual in that position brings more value to the role or could do more within their license.
Identify team role gaps and determine an action plan to fill them
Finally, determine the cost of realizing the new team design. Prioritize which roles may provide the most value in light of budgetary constraints.
Consider the following positions when mapping out the full team:
- Nurse practitioners and advanced practice nurses
- Physician assistants
- Mental and behavioral healthcare specialists
- Dietitians or nutrition specialists
- Clinical pharmacists
- Community health workers
- Social workers
- Ambulatory patient care technicians and assistants
- Collaborative care or care coordinator nurses
- Triage nurses
Once the team’s generalist clinical support positions are optimized, and tasks shift to other jobs, leaders can determine which roles could add further value.
An example of this transformation process comes from the Sigma Theta Tau nursing presentation referenced earlier. The Community Health Network of Indianapolis, Indiana, needed to re-envision its nursing workforce after the pandemic. Figure 2 demonstrates how the organization added new roles to its team-based model.
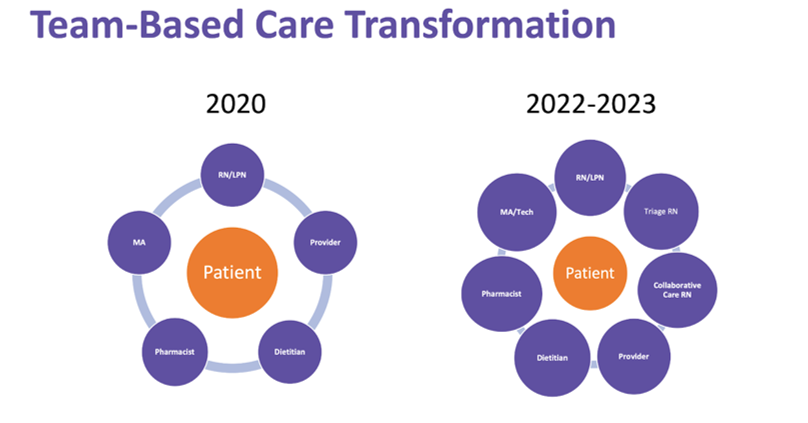
Figure 2: Closing the Gap: Team-Based Care Models. Presentation by Rackmil and Sego, nursing executives, for Sigma Theta Tau International, 2022.
Sigma Theta Tau increased efficiency with the new model. It enabled them to add care coordinators without adversely affecting their budget. They adopted a ratio of one RN care coordinator for every 2–4 full-time physicians.
Also, Allegheny Health Network (AHN) highlights the impact of transforming care to a team-based approach. AHN implemented a team-based primary care transformation process to enhance the quality and experience of care, improve population health, support clinician wellness and prepare for value-based reimbursement.
Their team-based model entailed three features:
- Core care team staffing consisting of physicians, advanced practice providers, nurses, medical assistants and health coaches
- Process improvement through learning collaboratives and practice coaching from transformation specialists
- Integration of behavioral health consultants, pharmacists, and registered dietitians into the care team
Beginning in September 2017 and continuing into early 2024, 10-12 practices within AHN launched a transformation project in three phases, including:
- Phase 1 – Optimize staffing by creating a core consistent care team
- Phase 2 – Process improvement focused on quality improvement methodology, pre-visit planning, population health outreach, access and care management
- Phase 3 – Introduce extended care teams (ECTs) based on a defined ratio of patient panel size, including clinical pharmacists, behavioral health consultants and registered dietitians
They monitored their performance—or return on investment—through enhanced value-based reimbursement (VBR), fee-for-service reimbursement for BHC services and improved transitional care management billing.
This initiative improved AHN’s Star rating for their large Medicare Advantage payor customers, as well as the aggregate Star rating across all AHN practices. Their rating exceeded the 4.5 threshold needed to trigger a superior performance bonus.
The resulting earnings of $983,000 were in addition to their base VBR earnings, as well as realizing unbudgeted bonus earnings. This ensured the program exceeded the annual investment in staffing and program support, achieving a significant return on investment.
Tapping the value of team-based care coordination
There are measurable benefits to improving how a care team is constructed and how functions are assigned. When each member is working at the top of their license, patient care achieves new levels of efficiency, engagement and wellness.
How ThoroughCare can help
Healthcare organizations use ThoroughCare to deliver integrated care management services to foster patient engagement and enhance revenue. Our platform provides the digital infrastructure to leverage fee-for-service programs for value-based success.
With seamless EHR integration and data interoperability across health information exchanges and remote devices, our platform supports solutions for:
- Chronic disease management
- Remote patient monitoring
- Behavioral health services
- Wellness assessments
- Transitional care
Providers use ThoroughCare to seamlessly manage populations, capture and act on patient data with interactive care planning and assessments, and visualize business performance to inform decision-makers.



