Making Care Primary: CMS’s New Value-based Initiative
This month, the Centers for Medicare & Medicaid Services (CMS) announced a new advanced primary care program. Called the Making Care Primary (MCP) Model, this new initiative will be tested in eight states over the course of 10.5 years, starting July 1, 2024.
These eight states include Colorado, Massachusetts, Minnesota, New Jersey, New Mexico, New York, North Carolina, and Washington, with plans to expand elsewhere.
The Making Care Primary Model has three goals
The program’s goals are threefold:
- Strengthen primary care
- Make value-based care contracts more attractive and feasible for primary care organizations and practices
- Improve care quality and patient health outcomes while decreasing care costs
Related to primary care delivery, MCP’s objective is to ensure that primary care is more integrated, coordinated, person-centered, as well as accountable.
MCP focuses on team-based care models, including care management, integration, and addressing health-related social needs (HRSNs) through community connections.
The program will be open to any Medicare-enrolled legal entity with a minimum of 125 attributed Medicare beneficiaries and at least 51% of primary care sites within an MCP state. It is intended to provide additional support to small, independent, rural, and safety net organizations, enabling them to enter into value-based care arrangements.
What is new about the Making Care Primary Model?
Building on previous primary care models like Comprehensive Primary Care (CPC), CPC+, Primary Care First, and the Maryland Primary Care Program (MDPCP), the MCP model has distinct differences that could make value-based care much more attractive for primary care practices and practitioners.
Difference #1 – Additional revenue to build infrastructure
CMS will support investment into care integration and care management capabilities for chronic disease management and behavioral health services, and to enhance healthcare access for rural residents. This investment will include tools for practices to partner with specialists and community-based organizations.
Through this investment, primary care teams can better address chronic disease.
Difference #2 – Flexible multi-payer alignment strategy
CMS’s goal is to reduce barriers and complexities for providers to join value-based arrangements. Their key to success is connecting the new MCP program to various health plans, including members covered by Medicaid, commercial plans, and other payers.
CMS will work with state Medicaid agencies in the first eight test states, but it plans to engage private payers as well. Because a mix of healthcare payers can influence provider behavior, the MCP program looks to flexibly align across multiple payers.
This could benefit primary care clinicians with improvements in care delivery, financial investments in primary care, and learning tools.
For example, Massachusetts has transitioned 85% of Medicaid-covered lives into accountable care since 2018. They have more than 1.3 million beneficiaries in an accountable care organization (ACO) and, in 2023, more than 1,000 primary care practices are receiving proactive primary care payments.
Difference #3 – Longer model testing time frame
The MCP Model will provide participants with additional revenue to build infrastructure, make primary care services more accessible, and enable coordination with specialists by implementing over a longer timeline.
The MCP program will run for 10.5 years, from July 1, 2024, to December 31, 2034, making it one of the most prolonged Center for Medicare and Medicaid Innovation (CMMI) initiatives.
Rollout to other states is expected once the first eight states launch and achieve critical milestones.
Difference #4 – Focus on reducing physician burden
Part of the reason 75% of primary care practices are not engaged in value-based arrangements is the complexity and the burden it can put on already-overwhelmed physician leaders.
The goal of the MCP program, according to CMS, “provides a pathway for primary care clinicians with varying levels of experience in value-based care to gradually adopt prospective, population-based payments while building infrastructure to improve behavioral health and specialty integration and drive equitable access to care.”
State Medicaid agencies are currently designing Medicaid programs to align with MCP in critical areas to support physician leaders financially, operationally, and technically.
By offering three tracks, the MCP model meets practices where they are and provides support so that tools and processes are easier to adopt for care management, specialist engagement, and community partnerships.
Difference #5 – Health equity strategy inclusion
New CMS models of care are beginning to include health equity, as was done with ACO REACH, the first model to incorporate health equity requirements.
CMMI believes that “equitable care is crucial to achieving high-quality care for Medicare and Medicaid beneficiaries” and is critical to MCP’s success.
The MCP Model features several components designed to improve health equity, including:
- Offering risk-adjusted payments
- Developing a strategic plan for identifying disparities and reducing them
- Implementing HRSN screening and referrals
- Reducing cost-sharing for patients in need
- Measuring the percentage of patients screened for HRSNs
Making Care Primary uses a progressive three-track approach to transformation
Participants in all three tracks will receive enhanced payments.
Those in Track One will focus on building infrastructure to support care transformation, like chronic care management. Tracks Two and Three will include certain advance payments and more opportunities for performance-based bonus payments.
By supporting practices across the value-based care readiness continuum, MCP will work to reduce organizations’ reliance on fee-for-service (FFS) payments.
Risk-adjusted enhanced services payments—also paid prospectively—will enable practices to implement or expand care management, screen for health-related social needs, and integrate with specialty care.
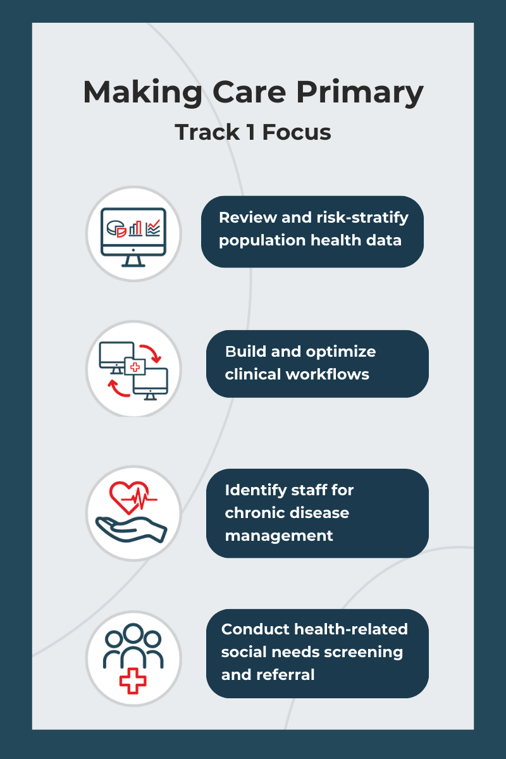
Track 1 Focus
While payment for primary care will remain fee-for-service, CMS will provide additional financial support so that practices can develop the necessary care transformation infrastructure and build advanced care delivery capabilities.
Participants can earn financial incentives for improving health outcomes without previous value-based care experience.
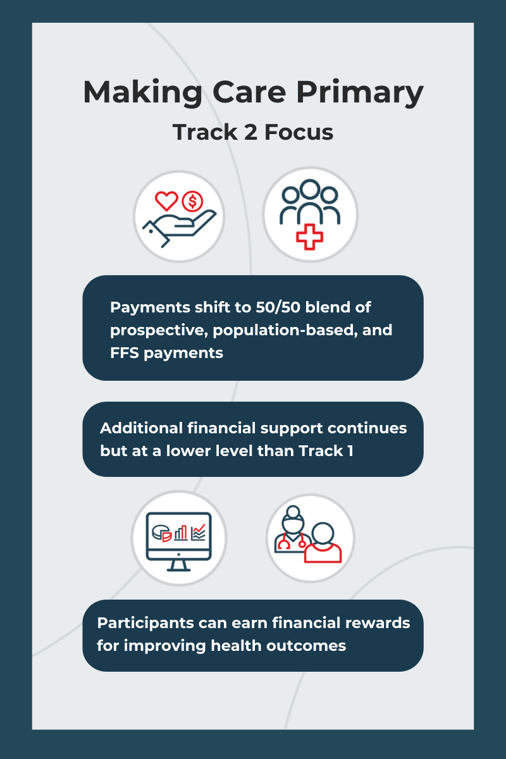
Track 2 Focus
Building upon the Track 1 requirements, Track 2 asks practices to partner with social service providers and specialists, implement care management services, and consistently screen for behavioral health conditions.
Track 3 Focus
Track 3 asks practices to analyze care quality data to determine ways of improving.
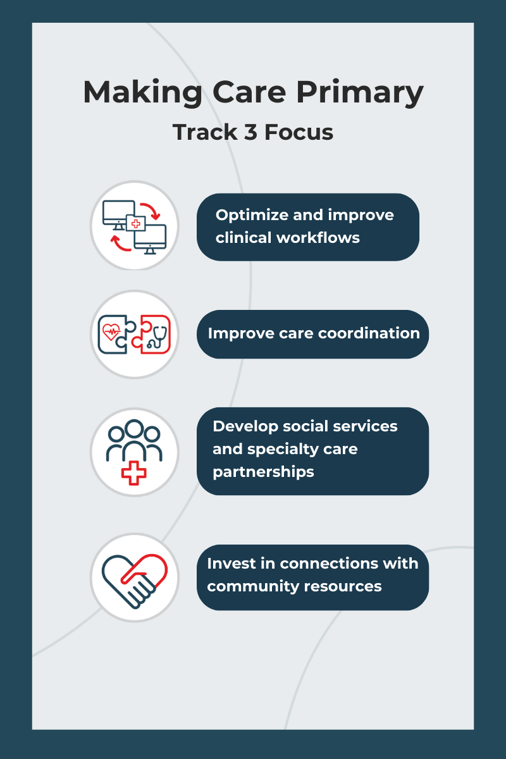
Payment shifts to entirely prospective, population-based payments.
Additional financial support continues, but at a lower level than Track 2, and financial rewards for improving health outcomes continue.
Making Care Primary launches July 2024
During the summer of 2023, CMS plans to release a Request for Applications (RFA) and provide technical details on the model design. Additionally, state Medicaid agencies should announce their individual state’s eligibility specifics in the same timeframe.
How ThoroughCare Can Help
More than 600 providers use ThoroughCare to manage and coordinate care. With seamless EHR integration and data interoperability across health information exchanges and remote devices, our platform supports solutions for:
- Chronic disease management
- Remote patient monitoring
- Behavioral health services
- Wellness assessments
- Transitional care
Providers use ThoroughCare to seamlessly manage patient populations, create and maintain holistic patient records with interactive care planning, motivate proactive engagement, and visualize and interpret data to inform care decisions.




