Annual Wellness Visit | CPT codes
2025 Medicare Annual Wellness Visit CPT Codes: G0402, G0438, G0439
What is a Medicare Annual Wellness Visit?
A Medicare Annual Wellness Visit (AWV) is a preventive screening used to identify gaps in care.
As covered by Medicare Part B, providers should understand what CPT billing codes matter to the service and how to use them. This can help your organization avoid denied claims and enhance care.
AWVs are covered for Medicare Part B patients without a co-pay. This yearly assessment helps patients create personalized care plans that providers can use to improve outcomes.
AWVs are reimbursable under Medicare’s Physician Fee Schedule, paying various rates.
Annual Wellness Visit CPT codes: G0402, G0438, G0439
Different CPT billing codes reflect specific types of Medicare wellness visits. The crucial qualifying determinant is when a certain AWV can be provided and billed for.
There are three types of wellness visits: Initial Preventive Physical Examination (IPPE), an Initial Annual Wellness Visit, and the Subsequent Annual Wellness Visit. Each entails a different billing code as well as specific qualifiers for each program.
CPT code G0402 description
- Initial Preventive Physical Examination (G0402): Patients may only receive this benefit within the first 12 months of their Medicare enrollment. Commonly referred to as the “welcome to Medicare visit,” it is considered a once in a lifetime assessment and after the initial eligibility period, the patient cannot receive an Initial Preventive Physical Examination. It is also dependent on the health risk assessment.
CPT code G0438 description
- Initial Annual Wellness Visits (G0438): Similar to an Initial Preventive Physical Examination, except it is available to a patient after 11 months of Medicare enrollment. This is for patients that miss their window for an Initial Preventive Physical Examination. However, if the patient does complete an Initial Preventive Physical Examination, they must still complete the Initial Annual Wellness Visit. This screening also includes an optional cognitive exam and end-of-life planning.
CPT code G0439 description
- Subsequent Annual Wellness Visit (G0439): Is the yearly follow-up to an Initial Annual Wellness Visit. Eleven full months after the Initial Annual Wellness Visit, a patient can attend these visits to modify and maintain their preventive care plan, based on how their health is at any given time.
Medicare Annual Wellness Visit guidelines
Medicare’s wellness visit is a yearly assessment of a patient’s health used to identify risks and create a personalized care plan. AWVs are different from yearly physical examinations. They offer a more complete review of a patient’s medical history and current lifestyle to suggest care goals that close gaps.
Wellness visits can be of particular importance for patients living with chronic conditions.
With an AWV, a personalized care plan is designed to help manage chronic illnesses, as well as schedule preventive screenings to improve early detection of disease.
Who can provide AWVs?
AWV billing must be directed by a provider with an NPI number. However, clinical staff can administer most of the assessment, saving physician time and involvement. Eligible providers include:
- Physicians
- Physician assistants
- Nurse practitioners
- Certified nurse midwives
- Clinical nurse specialists
- Pharmacists
AWV billing requirements
The following components must be included in a patient’s wellness visit:
- A health risk assessment
- A review and update of medical and family history
- A review of current providers, prescriptions/medications, and durable medical equipment suppliers
- Height, weight, blood pressure, BMI, and other routine measurements
- Personalized health advice, health education, and preventative counseling
- A list of identified risk factors, current medical and mental health conditions, and recommended treatment options
- A cognitive impairment screening
- A five to 10-year screening schedule for appropriate preventive services
- A review of the patient’s functional ability and level of safety, including screening for hearing impairments, risk of falling, activities of daily living, and level of home safety
- Identification of patients at risk for alcohol, tobacco, and opioid abuse
- Advance care planning
Submitting claims and Annual Wellness Visit ICD-10
Five items are required when submitting a Medicare claim:
- A CPT Code for the specific type of AWV provided
- An ICD-10 code for a general adult medical examination (Z00.00)
- Date of service
- Place of service (most office in-office or telehealth)
- Submit NPI number
It is helpful to know the staff care coordinator assigned to a patient in case of an audit.
Three steps to bill for AWVs:
- Verify CMS requirements were met
- Submit claims to CMS annually (or when best for your organization)
- Determine there are no conflicting billing codes
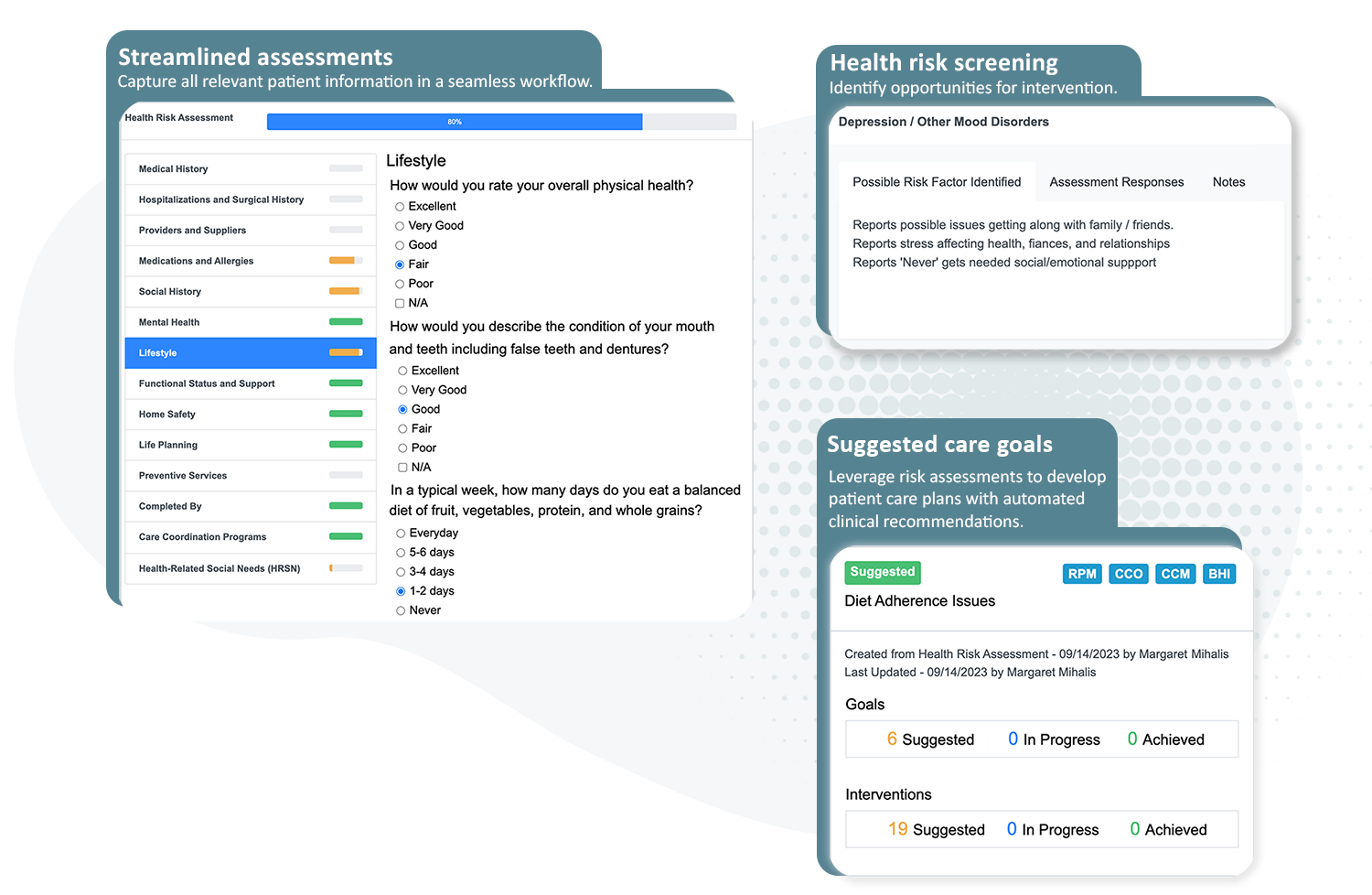
Identify risk: ThoroughCare helps clinicians deliver AWVs and close gaps in care
Annual Wellness Visits promote value-based care
AWVs ask about lifestyle, social history, mental health and home environment. Documenting these details can help providers risk-stratify patient populations and develop comprehensive, personalized care plans that can close gaps.
This can help clinicians better coordinate services, streamline collaborative decision-making and support value-based care delivery. AWVs have been shown to build stronger provider-patient relationships, secure additional revenue and contribute to cost savings.
Additional services to offer with AWVs
Medicare supports additional CPT codes for optional, add-on services related to AWVs. These include Advance Care Planning and a social determinants of health screening.
Advance Care Planning
Advance Care Planning helps patients prepare for future medical decision-making in case of serious illness or they are unable to communicate their care preferences. Specifically, Advance Care Planning includes two primary documents:
- A living will
- A durable healthcare power of attorney
An AWV assessment asks patients whether they have Advance Care Planning documents in place. If not, the provider can use the AWV to discuss advance care options and schedule time to complete a plan.
CPT code 99497
The average billing rate is $79.57. To accurately bill for code 99497, services must:
- Allow for 30 minutes of a face-to-face consultation with the patient, their family member(s), and/or a surrogate (with a minimum of 16 minutes of service time documented)
- Be provided by a physician or other qualified healthcare professional
- Include an explanation and review of advance care directives and options for completing them
Documentation to account for at least 16 minutes of service time should record that the ACP conversation was voluntary on behalf of the patient, encapsulate what was talked about, record who was present for the conversation, and note the length of time for the consultation.
Again, it is not required to complete an advance care directive during ACP. Completion is only required if you’ve noted in your documentation that you’ve performed this task. However, when ACP is completed with an AWV, it is entirely covered for the patient.
CPT code 99498
This is simply an add-on billing code to allow for an additional 30 minutes of ACP services. The average reimbursement rate is $68.90. Requirements for billing this code include:
- Listing this billing claim separately in addition to the code for the primary consultation
- That a minimum of 16 minutes past the first 30 minutes is documented using the same documentation requirements noted above.
Social Determinants of Health assessment
Providers can collect social determinants of health (SDOH) data while performing an AWV. SDOH discussions should be between 5 and 15 minutes in length, and cover food and housing insecurities, transportation needs, and utility difficulties.
The SDOH risk assessment addresses factors that influence the diagnosis and treatment of patients’ medical conditions. While not designed as a screening, the assessment is tied to one or more known or suspected SDOH needs.
CPT code G0136
Providers can receive an additional $18.44 for assessing SDOH during an AWV. For the patient, this assessment is fully covered by Medicare when provided with an AWV.
To claim this CPT code, providers must:
- Deliver 5-15 minutes of SDOH discussion
- Not assess a patient more than every 6 months
- Administer a standardized, evidence-based SDOH risk assessment
Medicare stresses the importance of following up with patients about SDOH and working to connect them with available resources.
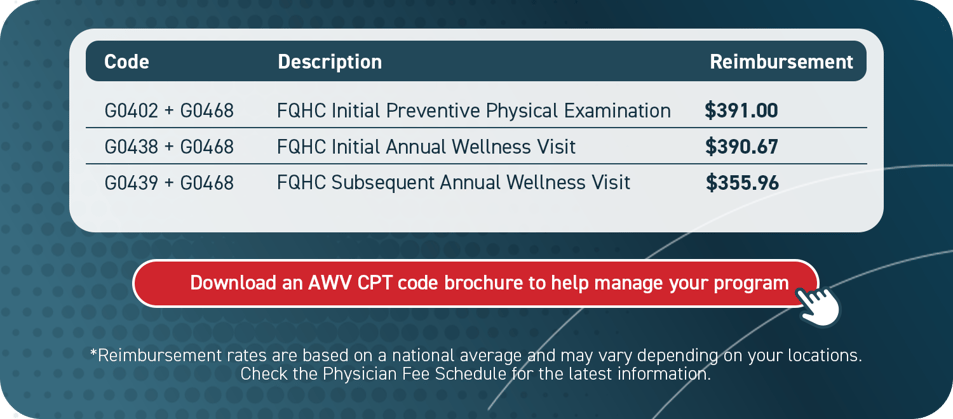
Medicare AWVs for Federally Qualified Health Centers
Federally Qualified Health Centers (FQHC) can bill for AWVs, but they utilize additional codes.
In addition to the standard CPT codes associated with AWVs, an FQHC may use a special add-on code (G0468) that will support additional reimbursement.
For example, if an FQHC were to provide an Initial Preventive Physical Examination, the clinic would bill for G0402 + G0468. This coding indicates to Medicare that the service is being provided through an FQHC.
These organizations receive much higher average reimbursement rates.
Maximizing the AWV with care management enrollment
Annual Wellness Visits can help enroll patients in care management programs, or provide additional assessments.
While there can be confusion around this opportunity, AWVs can be billed concurrently with problem visits, just not under the same code. Also, there are add-on services that can be billed concurrently, including:
- Advance Care Planning (CPT codes 99497 and 99498)
- Depression screening (CPT code G0444) – not permitted with the initial AWV, however.
- Smoking cessation counseling (CPT codes 99406 and 99407)
- Obesity counseling (CPT code G0447)
- Substance use disorder screening and counseling (CPT codes G0442 and G0443)
CMS also allows clinicians to enroll patients in Medicare care management programs during the AWV if they are eligible. The AWV is a great time to invite a patient into a care management program. It provides an invaluable service that supports a patient in realizing personalized health goals that align with the issues and risks discussed during the AWV.
Care management programs give the care plan structure, cadence and substance, making it actionable.
Which care management program is appropriate?
The table below outlines the general eligibility requirements for patients to join each of the Medicare care management programs. This matrix can help highlight which programs may fit your patient populations, indicating those programs you should consider offering during the AWV.
Program eligibility

To maximize the value of the AWV and enhance enrollment into care management programs, it helps to map out a workflow that indicates how you will engage patients before, during and after the yearly visit.
ThoroughCare simplifies Annual Wellness Visits
ThoroughCare gives providers the tools and support to make Annual Wellness Visits effective.
We help providers, based on their specific needs, build AWV programs or scale existing services. ThoroughCare supports a comprehensive software platform, clinical expertise to optimize workflows and assistance with data and reporting for quality improvement.
ThoroughCare includes digital solutions, such as:
- An interactive health risk assessment
- Screening tools, such as ADL, CAGE, DAST-10, GAD-7, MDQ, PAC, PHQ-2, and a mini cognitive exam
- A care gaps summary with recommended interventions
- A full report of Personalized Prevention Plan Services
- Comprehensive care planning tools
- Automated CPT code assignment for accurate billing
*Reimbursement rates are based on a national average and may vary depending on your location.
Check the Physician Fee Schedule for the latest information.


.jpg)