Care Coordination | Value-Based Care
Value-based Care Solutions: Health-related Social Needs
Unaddressed health-related social needs (HRSN) can make achieving care plan goals difficult.
Provider and payor organizations that assess, identify and work on HRSN can help remove barriers that would otherwise thwart clinical efforts. This can support more comprehensive patient care planning.
Care plan requirements of value-based care contracts, Medicare’s Chronic Care Management program, or other care coordination services aim to improve health outcomes, control costs and engage patients.
Integrating social needs into an existing care management or value-based care program
Practically, there are six phases along a continuum of identifying and addressing HRSN. Healthcare teams must decide how deep into each stage they can manage based on the overall level of risk and patient need.
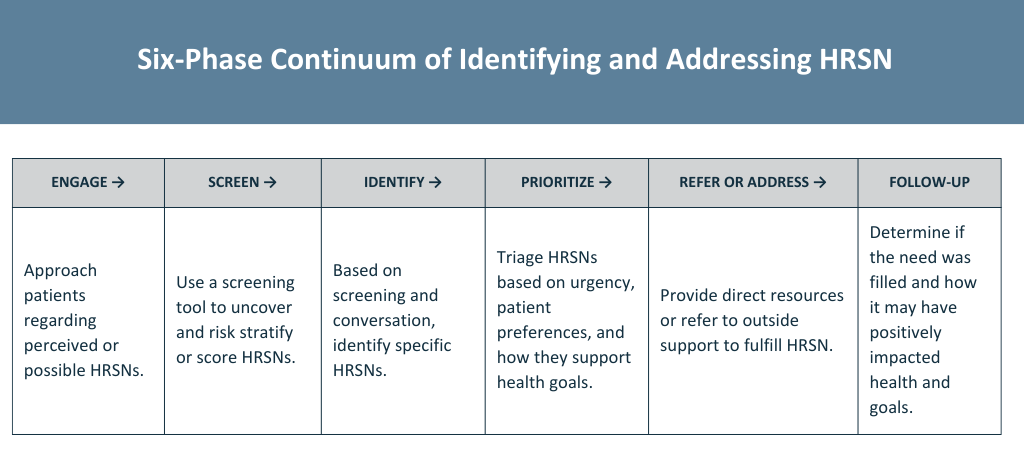 Six phases to identify health related social needs.
Six phases to identify health related social needs.
Existing value-based, team-based or care management programs should have existing workflows for enrollment, initial engagement, care planning and ongoing communication around progress and problem-solving.
A care team can decide where it may be appropriate to address possible health-related social needs.
The cycle above could start as part of an initial intake process, during care planning (as part of exploring possible barriers) or during progress discussions as challenges arise.
How broad and deep should HRSN services go?
At a high level, the payor or provider organization should decide how far they can or should go to address HRSNs once identified.
There are three approaches to how extensive an HRSN offering could become:
- Screen for HRSNs and provide a list of resources
- Screen and provide information but also help the patient connect with those resources
- Screen for needs but also provide direct resource support
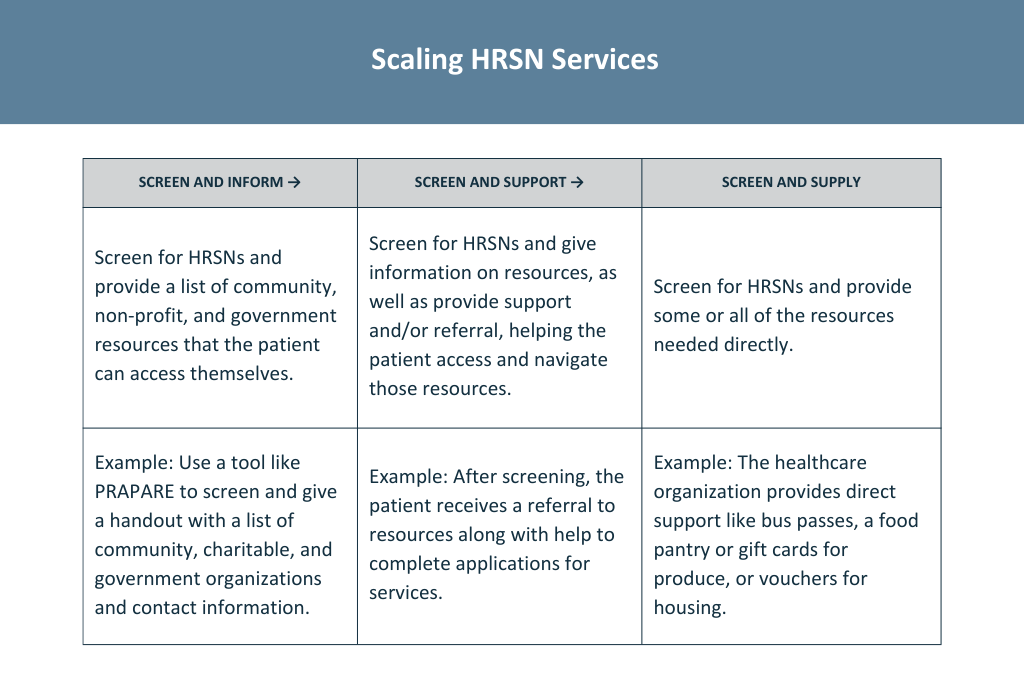
Examples of how to provide social needs services for a provider organization.
Healthcare organizations can decide to provide patient-level interventions to specific individuals from traditionally high-risk groups or offer practice-level interventions to all patients.
The difference relates to how the care team identifies people who may have health-related social needs. The team could opt to screen every patient or look for signals of HRSNs during regular appointments. It could also create a list of at-risk patients by analyzing a Chronic Care Management program and engaging them about HRSNs.
Beyond screening, each healthcare organization, program or care coordination team must decide if they have the capacity to inform, support or supply.
Some groups may start with informing and evolve into levels of navigation support, or providing some type of direct support in extreme cases. Or, the team may decide to educate every patient and support those at a higher risk level.
The breadth and depth can evolve as the team becomes more comfortable, or after piloting an HRSN program yields positive outcomes.
Building, piloting and scaling an HRSN initiative
What does it take to create a social needs initiative?
As mentioned previously, it requires having a sense of the level of need among a patient population. Or, there’s a desire to assess specific groups of patients to determine what types of HRSN assistance would be most impactful.
Alternatively, providers can use screenings or surveys to see what social needs emerge. Then, based on existing programs or staff, address specific needs.
However, several fundamental areas require thought, planning and action when establishing a process, including:
- HRSN screening tool, such as the Protocol for Responding to & Assessing Patients’ Assets, Risks & Experiences (PRAPARE)
- Staff training
- Integrated workflow
- Operational standards and processes
- Resource research
- Community referral structure
- Data exchange
- Communication and follow-up
Primary care HRSN case study
A case study of how the Lincoln Community Health Center implemented a health-related social needs program was published in the New England Journal of Medicine’s “Catalyst: Innovations in Care Delivery.” Their initiative improved care quality by measuring and responding to upstream social and economic risk factors disproportionately affecting low-income households.
HRSN Operations: Lincoln’s HRSN clinical workflow consisted of two distinct channels: (1) assessing needs with the use of the PRAPARE screening tool and (2) responding to needs via internal resources and/or through linkages to community-based organizations and social service agencies.
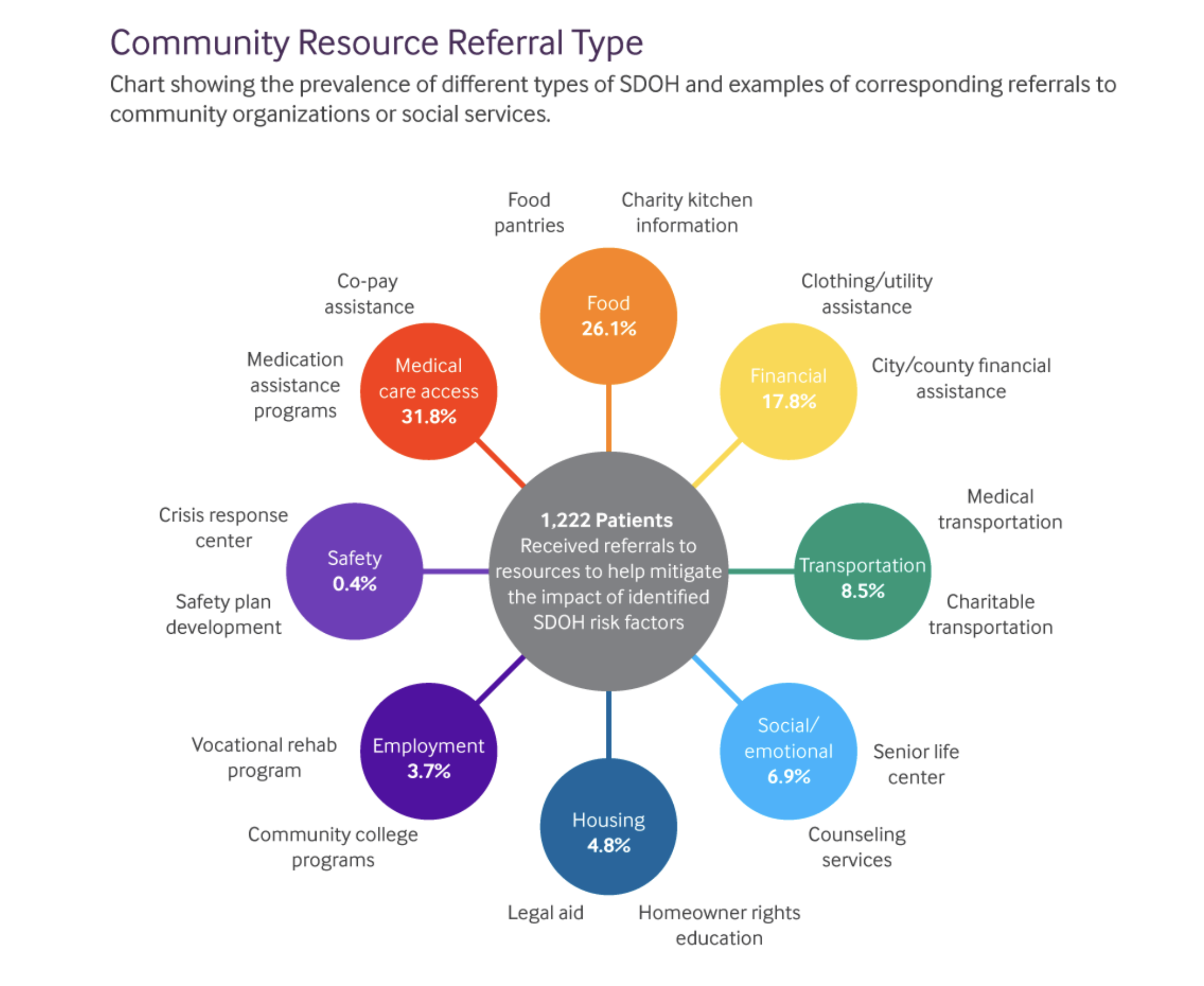 Data representing community resource referrals.
Data representing community resource referrals.
Source: Assessing and Addressing Social Needs in Primary Care.
HRSN Investment: The Lincoln team invested in staff training and time along with technology infrastructure that facilitated collection, documentation, analysis and action. They also conducted an environmental scan of appropriate local, state and federal resources, so that they could implement external referrals.
HRSN Team: Lincoln utilized a social worker case manager to conduct the PRAPARE assessment during or after clinical encounters. They prioritized engaging patients in person to explain why assessing non-medical needs allows the clinic to better serve and support them, rather than a self-administered tool.
HRSN Outcomes: Using an HRSN screening tool, the Lincoln team learned that “the most commonly reported affordability challenge that patients faced was related to medicine and medical care.”
Despite Lincoln being a federally qualified health center (FQHC) and offering a sliding fee scale, patients still struggled to pay for medications and medical care. Food insecurity was found in 30% of patient homes.
Patients who were found to have housing insecurity typically presented with a much higher risk profile since lack of housing presents many other health challenges. They also discovered that unemployment affected 13% of patients screened, as well as isolation, which affected about 25%.
Based on this data, the clinic prioritized what support they could give and which community resources they would refer to. The figure below shows the percentage of patients facing each type of need.
The team also created a reference to identify community resources aligned with specific risk factors and PRAPARE questions, as shown below.
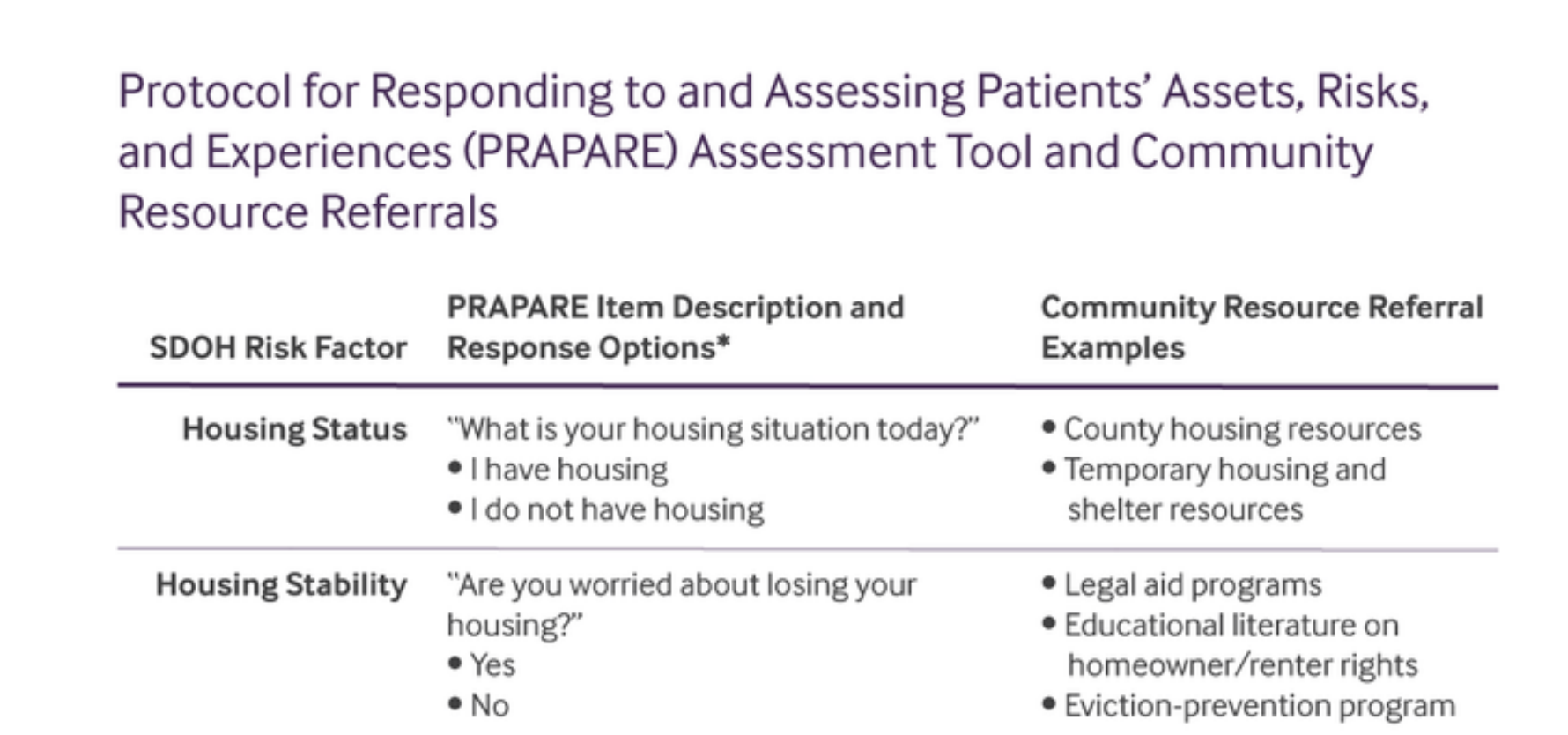 Some of the program designs used for the Lincoln Community Health Center case study.
Some of the program designs used for the Lincoln Community Health Center case study.
Source: Assessing and Addressing Social Needs in Primary Care.
Lincoln’s approach shows one potential program designed to help patient populations address social needs. It provides rich insight into the types of support their patients need most.
Tailoring HRSN supports for patient-centered care planning
There are many options for how to pilot and implement a health-related social needs initiative.
The key to creating a sustainable and scalable program is to align staff capacity, community resources and patient needs.
When integrated with an existing care management or value-based care program, addressing HRSN can maximize existing clinical and non-medical support toward better outcomes.
Selecting a health-related social needs screening tool
Screening for health-related social needs is evolving into a care standard. Value-based care contracts and accreditation bodies are beginning to require screening for social determinants of health and social needs.
The Joint Commission now asks healthcare organizations to assess HRSNs for a representative sample of their patients. Their focus on health-related social needs highlights the needs of individuals versus social determinants of health that describe population characteristics and influences.
Health systems, ambulatory settings, and health plans will begin to see more screening requirements for HRSN or SDOH. However, most will leave the choice of which tool or questions to use up to the healthcare organization.
While there has been little research into health-related social needs or SDOH assessment tools, several have been validated and reviewed. These options are in alignment with the Institute of Medicine's (IOM) recommendations and other healthcare quality organizations' requirements.
Validated social needs and SDOH assessment tools
The following social needs assessment tools are among those provided as resources by the Joint Commission, along with many other screening support materials and education.
- The Health-Related Social Needs (HRSN) Screening Tool includes 10 items categorized into five domains: housing instability, food insecurity, transportation problems, utility help needs, and interpersonal safety. This tool leverages other validated assessments.
- The Protocol for Responding to and Assessing Patients’ Assets, Risks, and Experiences (PRAPARE) is a nationally standardized patient risk assessment protocol based on national core measures.
- Developed by a nonprofit organization founded by physicians and public health innovators, the HealthBegins screening tool assesses 12 domains and provides a minimum frequency for re-assessment.
- The American Academy of Family Physicians (AAFP) created an SDOH short form that includes 11 questions on housing, food, transportation, utilities, personal safety, and the level of assistance needed.
- AccessHealth created a social determinants screening tool as a companion to the Center for Health Care Strategies’ brief, Screening for Social Determinants of Health in Populations with Complex Needs: Implementation Considerations.
- CMS created the Accountable Health Communities Health-Related Social Needs Screening tool to assess needs in 5 core areas: housing instability, food insecurity, transportation problems, utility help needs, and interpersonal safety.
While some tools focus on a single social need area (i.e., food insecurity), others focus on multiple factors.
Vetting HRSN screening tools for care objectives
When vetting and implementing a screening tool, healthcare leaders should tailor it to meet the unique needs of their SDOH or care management program, patient population, and programmatic goals.
Consider these steps when adapting or adopting a screening tool:
- Confirm that questions are written at an accessible reading level for your patient population
- Pilot your chosen tool before committing to it or scaling its use to more programs or populations
- Consider the published research on individual instruments and vet those tools with your clinical and program leaders
- Ensure that the new tool doesn’t overlap with existing surveys or EMR questions to avoid redundant data collection
- Integrate your chosen social needs screening tool into existing clinical and care management workflows
- Capture screening data in digital form through your EMR or care management platform
ThoroughCare ties HRSN to care management
Healthcare organizations use ThoroughCare to deliver integrated care management services to foster patient engagement and enhance revenue. Our platform provides the digital infrastructure to leverage fee-for-service programs for value-based success.
With seamless EHR integration and data interoperability across health information exchanges and remote devices, our platform supports solutions for:
- Chronic disease management
- Remote patient monitoring
- Behavioral health services
- Wellness assessments
- Transitional care
Providers use ThoroughCare to seamlessly manage populations, capture and act on HRSN data through comprehensive care planning and assessments, and visualize business performance to inform decision-makers.



