Care Coordination | Care Management
How Care Management and Care Coordination Can Improve Star Ratings
Nearly 50% of Medicare beneficiaries are enrolled in Medicare Advantage plans. Each of those health plans is given a Star Rating, which has become the cornerstone of consumer rankings, performance assessment, and more than $12 billion in Quality Bonus Payments.
Care management and care coordination approaches hold significant value and potential to help payors and providers align with evolving Star Rating priorities. And, in light of post-pandemic Star Rating declines, healthcare organizations can leverage care management programs to improve health and financial outcomes.
What are Star Ratings?
Since 2007, the Stars Rating system has become a source for consumers to research and compare Medicare Advantage health plan options. It also established a scoring-based reward system comprised of composite performance scores on measures across nine domains, including:
- Health maintenance
- Chronic disease management
- Member experience
- Member complaints
- Customer service
- Plus, four additional domains for Part D plans regarding drug coverage
Figure 1 shows how the rating is organized across four measurement categories.
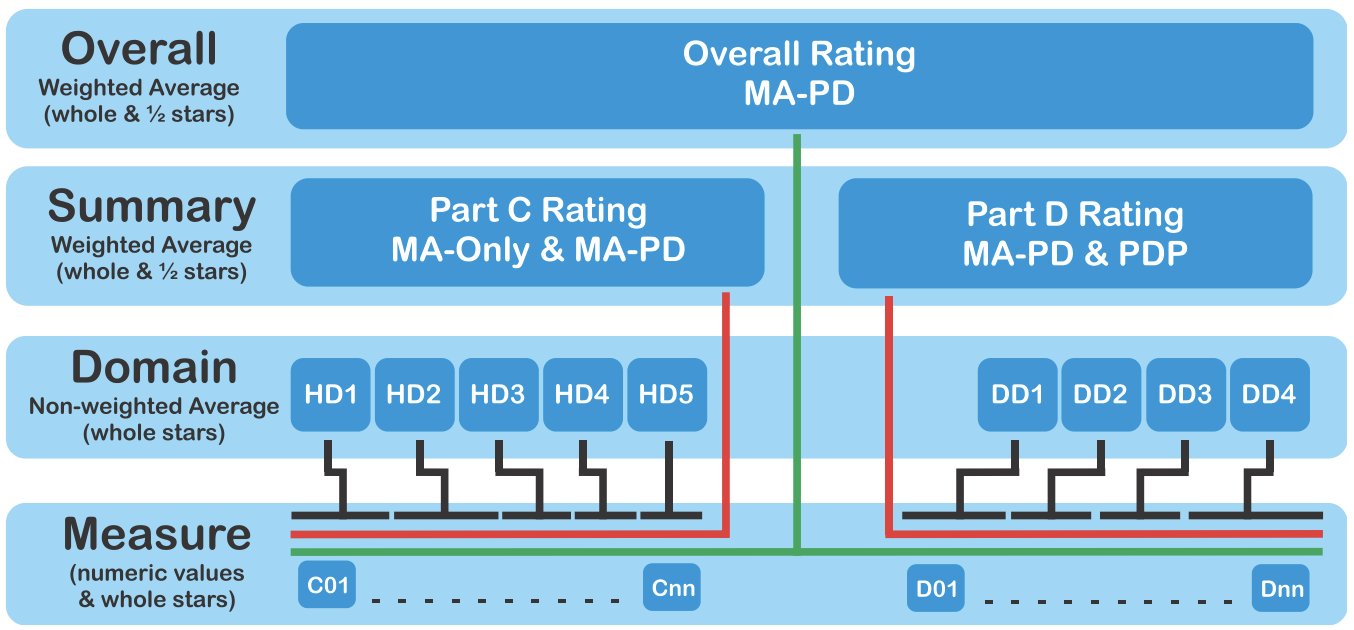
Figure 1: Medicare 2024 Part C & D Star Ratings Technical Notes
Star Rating scores range from one to five stars and are assigned to individual contracts within and across health plans. For 2024, 31 contracts received five stars, down from 57 in 2023, and four received just two stars.
The 40-plus clinical performance measures used to calculate Stars Ratings come from those developed and maintained through the following organizations and surveys:
- National Committee for Quality Assurance (NCQA)
- Healthcare Effectiveness and Information Set (HEDIS)
- Pharmacy Quality Alliance (PQA)
- CMS Health Outcomes Survey (HOS)
- Consumer Assessment of Healthcare Providers and Systems (CAHPS)
How Star Ratings affect payor and provider revenue
With more than $12 billion in Quality Bonus Payments at stake, Star Ratings directly affect health plan revenue and their network of providers.
Currently, QBP bonus and rebate percentages are based on the following Star Ratings schedule:
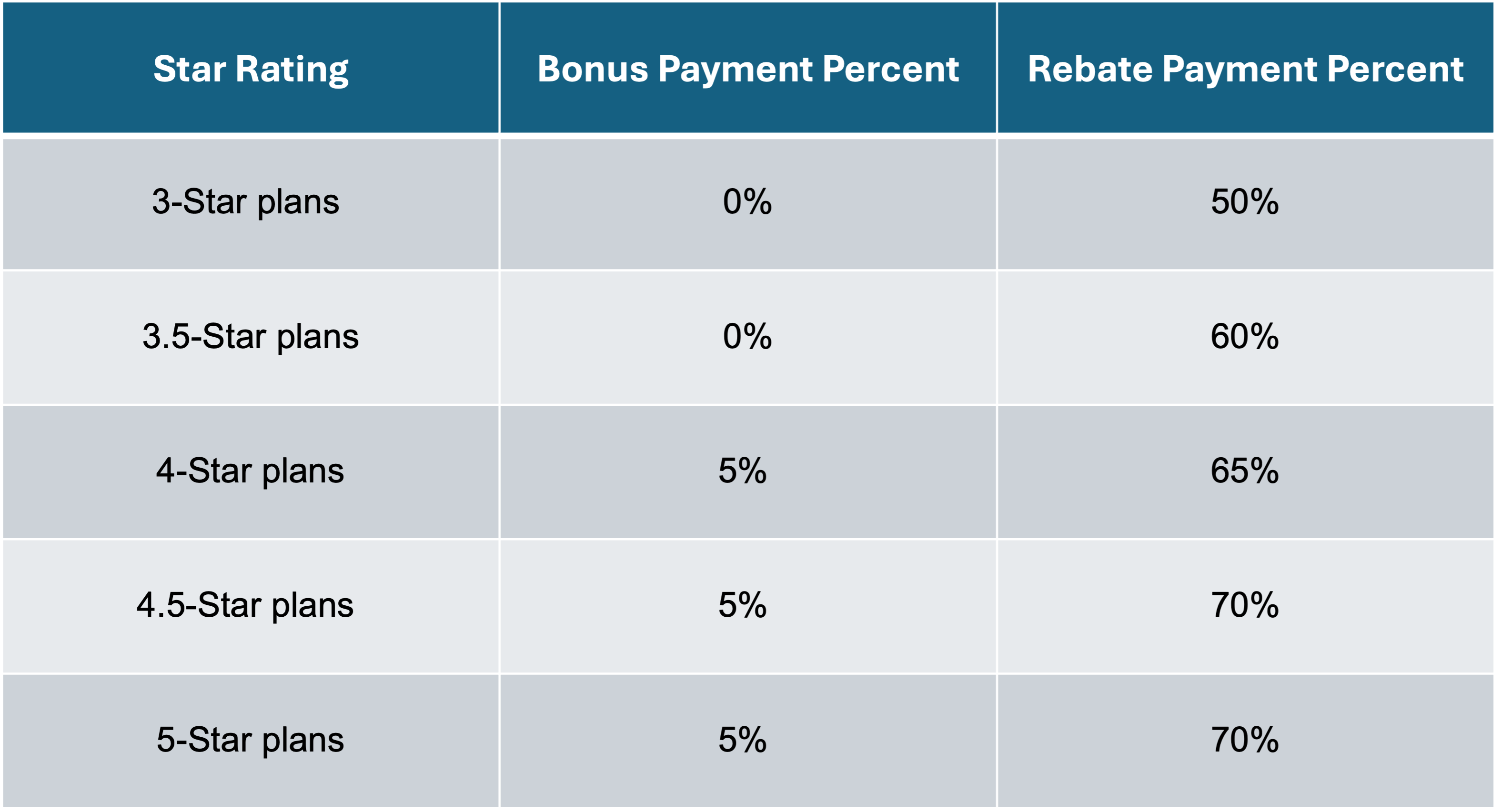
These rebates and bonus payments enable Medicare Advantage plans to offer additional benefits like Chronic Care Management, Transitional Care Management, Remote Patient Monitoring, and Behavioral Health Integration to stay competitive and reach growth and profitability targets.
A drop in a contract’s Star Rating could equal millions of dollars lost in payor revenues. In 2024, a decrease in 5-star plans resulted in more than $1.5 billion in lost Quality Bonus Payments. The average contract Star Rating decreased from 4.14 to 4.04.
Over the next decade, Star Ratings will be even more critical for payor and provider organizations as the Centers for Medicare & Medicaid Services (CMS) aims to save $2.2 billion.
Star Ratings reflect healthcare’s evolving priorities
Each year, CMS establishes the thresholds for five-star plans, and it adjusts measures based on trends and healthcare priorities that require inclusion or exclusion. As priorities shift or become weighted more heavily in the scoring, various healthcare areas and programs require greater focus.
For 2024, the Star Ratings methodology changed in material ways. For example, two new measures were introduced, including Transitions of Care (Part C) and Follow-Up after Emergency Department Visit for People with Multiple High-Risk Chronic Conditions (Part C) measures.
Also, the weight for the Part C Controlling Blood Pressure measure was increased from one to three, reflecting its rising importance in overall Star Ratings.
As we’ll see, the increase in comorbidities among Medicare Advantage members is causing payors and their provider networks to focus more on care management programs and enhanced coordinated care.
Care management and care coordination align with Star Ratings measures
Care management programs can address most of the Part C and Part D domains and quality measures.
Here is a sampling of the measures that care management programs – such as Chronic Care Management, Transitional Care Management, Behavioral Health Integration, and Remote Patient Monitoring – can support toward improved Star Ratings:
- Care Coordination
- Medication Adherence for Diabetes
- Medication Adherence for Hypertension
- Medication Adherence for Statins
- Follow-up After Emergency Department Visit for People with Multiple High-Risk Chronic Conditions
- Diabetes Care - Blood Sugar Controlled
- Controlling High Blood Pressure
- Medication Reconciliation Post-Discharge
- Plan All-Cause Readmissions
- Transitions of Care
- Colorectal Cancer Screening
- Annual Flu Vaccine
As this list shows, care management and payor performance go hand-in-hand.
An example of identifying and meeting specific quality measures
For example, a provider may want to identify members who do not currently receive statin therapy for cardiovascular disease or high blood pressure. They want to be proactive and ensure that members who would benefit from this treatment have access to it. Doing so helps the provider meet this specific quality measure.
By using a software platform, such as ThoroughCare, this identification can be simplified through analytics and reporting, all within a comprehensive dashboard. This gives providers a clear, quick view into who is missing this key measure and ensures care management efforts are targeted to the members who need it.
Five specific areas where a care management program can improve Star Ratings
Medication reconciliation and adherence
More than half of the Star Rating system is tied directly to medication-related management, which makes medication reconciliation a critical objective.
Aligning a member’s recommended medications with their current medications is central to any care management program. This ensures the member understands the role of each medication in their health.
Care management programs that engage members regularly provide consistent checks to assess adherence and determine if care, education, or social determinant barriers keep the member from taking their medication as prescribed.
Related to transitioning from an inpatient setting, the Medication Reconciliation Post Discharge (MRP) measure requires Medicare Advantage plans to oversee medication reconciliation for individuals within 30 days of discharge. This is to prevent avoidable hospital readmission and keep members healthier at home.
Payors with care management programs can partner with pharmacists to leverage their expertise as part of the care team. Through phone or telehealth contact, pharmacist-led interventions can be particularly valuable among high-risk members who have many medications to manage.
Transitions of care
Nearly 20% of Medicare beneficiaries discharged from the hospital were readmitted within 30 days, and 34% were readmitted within 90 days. These readmissions cost Medicare $17.4 billion annually.
Since 2022, transitions of care have become a prominent focus for Star Ratings, with CMS instituting measures that require:
- Notification of inpatient admission and documentation of receipt of notification of inpatient admission by the day following admission
- Receipt of discharge information and documentation of receipt of discharge information by the day after discharge
- Member engagement after inpatient discharge with evidence of contact with the member within 30 days of discharge, including an office visit, telehealth visit, or home visit
Transitional Care Management programs engage members at a critical time following hospital discharge.
Through remote and in-person interactions, clinical staff provide a combination of assessment, education, referrals, and support with regimen adherence, medication management, and community services.
Enhance chronic condition management
A prominent feature of Star Ratings is its consideration of measures related to managing chronic conditions, which are prevalent among Medicare beneficiaries.
The key to maintaining or improving ratings is to provide personalized, long-term health management support that streamlines care, closes gaps, and addresses social and clinical determinants.
Care management programs such as Chronic Care Management, Remote Patient Monitoring, and Behavioral Health Integration were built around the specific needs of at-risk members with comorbidities.
Through ongoing assessments, personalized care plans, continuous patient monitoring, and behavior-driven goal setting, care teams can improve health outcomes relevant to Star Ratings and avoid unnecessary and costly care that reduces overall scores.
Engagement and experience
The Consumer Assessment of Healthcare Providers and Systems (CAHPS) survey accounts for nearly a third of Star Ratings, and member engagement and experience are at the center.
Care management programs emphasize whole-person care. They leverage motivational interviewing, SMART goals, and individualized education to engage a person’s life and health objectives.
Through preventive screenings, health risk assessments, and social determinants of health surveys, care managers provide a person-centric experience and bridge care among various channels.
A 2022 BCG study revealed that health plans implementing personalization saw member experience scores improve by 10%. They also saw administrative costs decrease by 5-10% and quality standards increase by 20-25%.
One of the most valuable aspects of care management programs is their ability to provide regular and personal member engagement and consistent follow-up. Tapping into a member’s motivation and providing proactive communication and education help support and activate member participation.
Lastly, care managers can help assuage provider attention and communication concerns by acting as a bridge and problem solver.
Social determinants of health and overcoming care barriers
Like many healthcare initiatives and directives, social determinants of health are growing in influence on Star Ratings. In direct and indirect ways, health-related barriers to care dramatically influence a payor’s ability to support members, as seen in Star Rating measures like preventative care, chronic disease management, and medication adherence.
New coverage for an optional SDOH health risk assessment, as part of the Medicare Annual Wellness Visit, provides an opportunity to uncover and address barriers. A wellness visit can also help providers enroll members in care management programs that meet the needs prioritized within Star Rating measures.
ThoroughCare streamlines care management programs
Meeting the evolving priorities represented within Star Ratings measures can be challenging. However, several care management programs empower payors and their provider partners to improve outcomes that impact revenue.
ThoroughCare is a comprehensive software platform that supports end-to-end workflow and simplified billing for care management. ThoroughCare provides a structured approach while enabling flexibility to meet individual patient needs. This includes:
- Enrolling new patient participants in care management programs
- Creating and maintaining comprehensive patient care plans
- Meeting and tracking program requirements
- Automating time-based claims documentation for auditing
- Assessing patient symptoms, condition barriers, and care goals to determine planned interventions



