How Providers and Health Plans are Reducing Hospital Readmissions
Ineffective transitions of care challenge providers
Readmission rates have remained high despite the Hospital Readmission Reduction Program (HRRP). The average US all-cause readmission rate is 14.56%, and it ranges from 11.2% to 22.3% across states. Other value-based care programs, where reimbursement is tied to the quality of service, haven’t led to a significant change in readmissions, either.
The Centers for Medicare and Medicaid Services (CMS) estimates that it spends $17 billion annually on avoidable hospital visits.
Frederick Bloom, MD, Family Medicine physician and Chief Population Health Officer at Guthrie Clinic, one of the nation's first multispecialty group practices, recently shared on a Becker’s Health webinar that the goal of managing care transitions is to “get patients home safely.” To keep them there.
Research and discussions, such as the Becker webinar panel, demonstrate real-world ways that provider organizations and health plans are working collaboratively to reduce readmissions.
Care transitions require a comprehensive approach
Research has shown that interventions involving multiple components have successfully reduced readmission rates for patients discharged home. That same research highlighted the types of activities that have the most impact. Additionally, it showed that using a single component was unlikely to reduce readmissions significantly.
Key activities that had the most impact when combined included:
- Patient needs assessment
- Medication reconciliation
- Patient education
- Arranging timely outpatient appointments
- Providing telephone follow-up
According to our partner, PointClickCare, “Evidence has shown that providing multifaceted intervention bundles, which include components such as pre-discharge patient education, implementation of a discharge checklist, medication reconciliation, and post-discharge follow-up, are necessary to decrease readmission rates.”
However, as the panel of health plans, provider leaders, and physicians attested in the Becker webinar, close collaboration and cooperation among health plans, hospitals, post-acute care centers, and family caregivers are critical. This can help avoid readmissions and reduce decomposition, preventable adverse events, and medical errors.
Real-world success: Provider-health plan collaboration, coordination, and communication
Figure 1 emphasizes the key transition points as a patient shifts from inpatient care to an outpatient facility, their home, or a long-term care facility. This requires continued follow-up through post-acute care with their PCP or specialist.
Figure 1: Transitions of Care Continuum including major points of care as a patient is discharged to home or a post-acute care facility.
During Becker’s "Optimizing Post-Acute Care: Collaborative Strategies for Payers and Providers" webinar, the panel offered examples of effective care transition strategies. These include:
Collaboration to reduce denials and streamline pre-authorization
Sarah Decaro, MD, VP and System Medical Director for Care Management at Emory Healthcare, points to delays of 24 hours to a week that cause longer stays and worsen patient outcomes before discharge. Working closely with health plans is essential to reduce denials and streamline pre-authorization for the next level of care.
Partnering with SNFs to overcome patient data and staffing issues
Fred Bloom, MD, Chief Population Health Officer at Guthrie Clinic, explained that they have implemented EHR instances in each nursing home. This allows SNF staff to access patient data seamlessly. They’ve also improved some SNF staffing issues by supplying providers for their patients. Lastly, they review readmission cases with nursing homes to discover causes and improve the quality of care.
Creating a bridge between acute and post-acute care
JP Holland, CEO of Johns Hopkins Health Plan, pointed to technology and people who act as a bridge between acute and post-acute care, including:
- Real-time communication platform
- Dedicated care coordinator roles
- Predictive analytics that flag risks early
- Remote Patient Monitoring can provide real-time recovery information
HIE integration and real-time communication
Howard Bill, senior vice president of Population Health at Monroe Plan for Medical Care, highlighted how HIE integration and real-time chat help with ongoing communication. He also emphasized the need for more technology, as it can promote greater interoperability and interactive communication between providers and the health plan.
Working with physicians to enhance PCP access
Adam Loris, CEO of Barstow Community Hospital, said they have trouble getting patients seen by primary care within 24 to 72 hours. They asked their referring physicians what could help, and learned they needed to create a discharge clinic staffed by a hospitalist. Through this model, they now support PCPs with medication orders, readmission reports, and points of contact.
Transitional care strategies that reduce readmissions
Webinar panelist Nicole Sunder is the senior director of solution design at PointClickCare. She spoke to the infrastructure landscape needed to build an acute-post-acute care network fully.
Figure 2 illustrates the various partners and transition points that would benefit from a single point of contact and interoperable technology.
Figure 2: Transitions of Care Continuum with infrastructure to connect partners sharing data, technology, and communication for improved coordination and patient experience.
Ideally, health plans and provider partners throughout the continuum work together to build a network of relationships, technology, data-sharing, and standards. All of these components help streamline communication, coordination, and the patient-caregiver experience.
In addition to the lessons learned and approaches shared by the webinar panel, here are five strategies that support transitional care and reduce readmissions through provider-health plan collaboration.
1. Interoperability
As shown in Figure 2, there are a number of points where technology aids in real-time access to patient data via interoperability, including:
- Inpatient discharge
- SNF admission
- Medical history
- Medications
- Recent lab results
- Clinical and risk assessments
With these details, care teams can make better, well-timed decisions, collaborate more effectively, avoid errors and reduce the risk of readmission.
An effective digital infrastructure should include:
Electronic Health Record (EHR): Central repository of medical history, clinical activity, and medical orders
Health Information Exchange (HIE): Secure electronic transmission of healthcare data across numerous organizations and sources
Application Programming Interface (API): Direct HIE feed via HL7 ADT messaging
Care Management Software: Specialized platform for standardized workflow, assessments, care coordination, and patient engagement activities
2. Dedicated transition roles
Dedicated roles for activities like discharge planning, care coordination, and care management are critical to effective care transitions.
Professionals, such as care managers, care coordinators, discharge nurses, social workers and pharmacists, provide collaborative points of contact among providers, patients, and their family caregivers.
These relationships, when streamlined with digital tools, are the backbone of effective care transitions.
3. Care management programs
Medicare care management programs, such as Transitional Care Management (TCM), offer a focused, personalized, and standardized workflow and support reimbursement. A TCM program includes:
- Evidence-based assessments
- Care tasks and plans
- Risk identification and mitigation
- Patient and family education and engagement
TCM has been shown to lower 90-day episode spending significantly, as well as emergency department visits, hospitalizations, readmissions, and 90-day mortality.
Hospitals that provide the following activities were most likely to offer a TCM program:
- Medication reconciliation
- Telephone or in-home follow-up
- Standardized processes for follow-up with primary and specialty care
- Timely sharing of discharge summaries
- Use of patient navigators, care managers, or health coaches following discharge
Figure 3: Transitions of Care Continuum noting where the Transition Care Management program plays a role post-discharge.
As shown in Figure 3, the TCM program is implemented at the point when the patient is discharged home or to a long-term care facility. It acts as a bridge between inpatient and post-acute care.
As a 30-day program, TCM reimburses for two CPT codes and requires three levels of contact, as shown in Figure 4.
Figure 4: Three types of timely contact required for Transitional Care Management.
In addition to TCM, other Medicare care management programs provide ongoing support for higher-risk patients or those with one or more chronic conditions. These programs include:
- Principal Care Management
- Chronic Care Management
- Advanced Primary Care Management
- Annual Wellness Visits
- Advance Care Planning
- Remote Patient Monitoring
4. Communications strategies
Building a network of relationships is also essential, in addition to having dedicated roles on the transitional care team and utilizing technology and data to collaborate.
Research has shown that inaccurate or untimely communication and ineffective teamwork are the leading causes of preventable adverse events, including medication errors, misdiagnosis, and readmissions.
Communication enables quality improvement. Teams that share data and collaborate can successfully intervene when problems arise.
Prioritizing regular reviews between leaders can uncover areas where additional technology, new standards of care, workflow steps, or data is needed.
5. Patient and caregiver engagement
Proactive engagement helps patients and their family caregivers understand the changes to their condition or medical regimen. This encourages the patient to self-manage and the caregiver to provide support.
Figure 5 highlights where care management programs can support patient and family education, as well as help connect them to community services vital to recovery and staying healthy.
Figure 5: Transitions of Care Continuum highlights how care management programs connect patients to community support services.
Digital tools can play a central role in providing access to approachable, evidence-based, multimedia education.
Other care management programs, such as Caregiver Training Services (CTS) and Guiding an Improved Dementia Experience (GUIDE), offer reimbursement for supporting family caregivers. They cover training for topics, such as clinical caregiver skills related to hands-on treatment, reducing complications, or monitoring the patient.
How ThoroughCare supports transitions of care
Provider organizations use ThoroughCare to deliver integrated care management services to reduce readmissions and mitigate post-discharge risks.
Our platform provides a digital infrastructure to deliver transitional care services, whether in compliance with Medicare’s TCM program or directly through other value-based or bundled payment contracts.
With seamless EHR integration and data interoperability across health information exchanges and remote devices, our platform supports solutions for:
- Chronic Care Management
- Remote Patient Monitoring
- Behavioral Health Integration
- Annual Wellness Visits
- Transitional Care Management
ThoroughCare offers robust functionality as well as dashboards, reports, and data visualizations critical to managing patient transitions and collaborative care.
TCM dashboard
This feature allows care teams to monitor the effectiveness of TCM services, optimize care coordination, and improve patient outcomes.
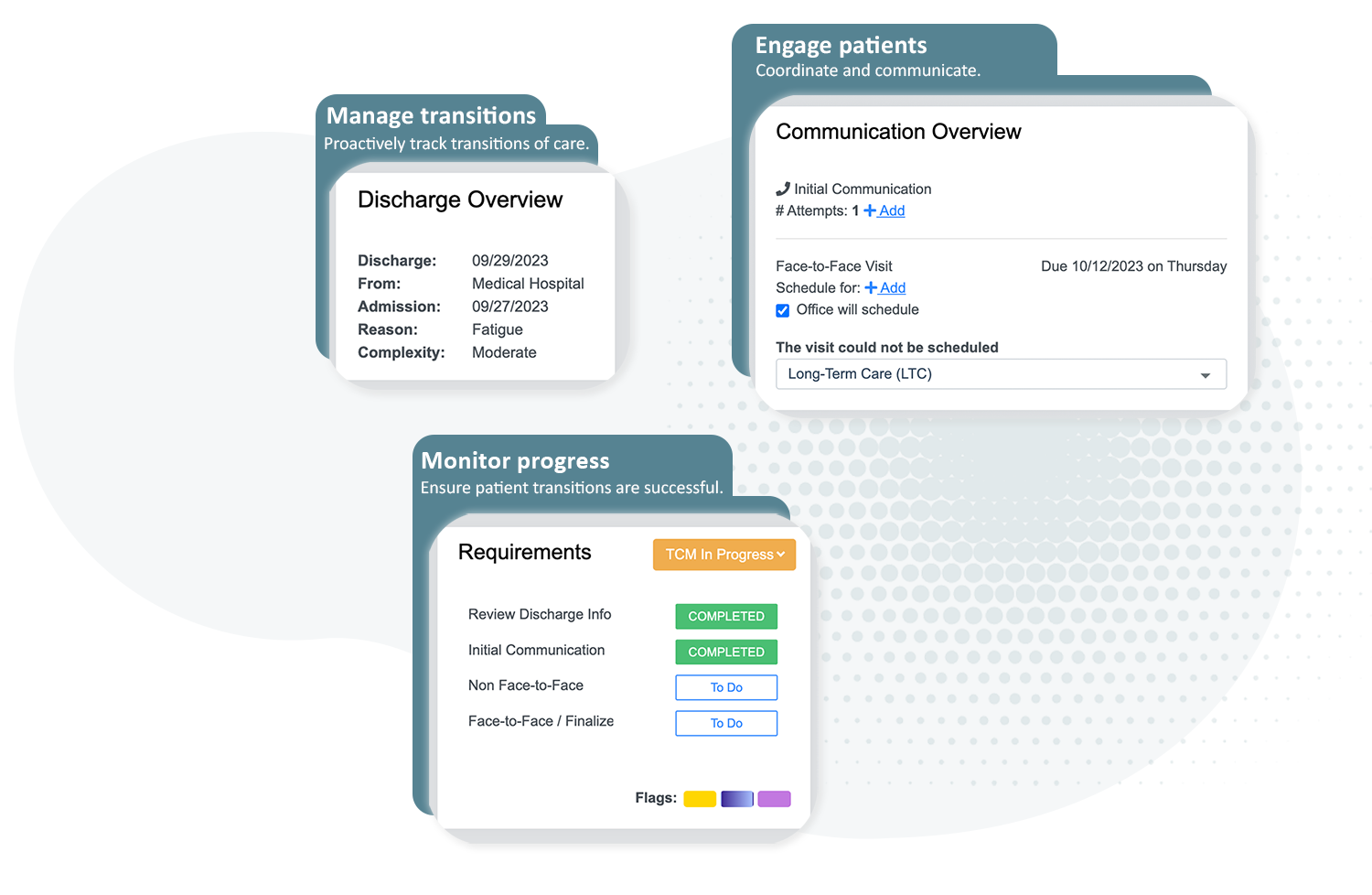
The Dashboard provides metrics to track monthly discharges, complexity, patient stage, and status.
Transitional care KPIs
ThoroughCare helps care managers oversee the entire TCM process, with easy-to-access data, including but not limited to:
- Number of patients discharged this month compared to last
- Number of patients in TCM categorized as low, moderate, and high complexity compared to last month
- Average number of TCM call attempts per patient before successful contact
- Percent of patients who’ve completed the TCM program
- Average number of days from the day the high-, moderate-, or low-complexity patient started TCM to their face-to-face visit
- Number of high-, moderate-, or low-complexity patients who have not yet had a face-to-face visit
Report visualizations
ThoroughCare provides a host of quick data visualizations to help the care team and leadership stay on top of all transition of care cases, including:
- Current patient status
- Top 5 reasons for incomplete TCM
- Top 10 discharging facilities this month
- Discharged to locations this month
Key questions answered
How can health plans and provider organizations collaborate more effectively to improve transitions of care and reduce readmissions?
There are a number of strategies that can be deployed to enhance healthcare collaboration before, during, and after a patient’s inpatient discharge to post-acute care, which include:
Using multiple interventions, such as combining patient needs assessment, medication reconciliation, patient education, arranging timely outpatient appointments, and providing telephone follow-up.
Additionally, transitional care teams have found the following strategies effective:
- Technology that supports interoperability and data sharing
- Dedicated transition care roles, such as care managers, care coordinators, discharge nurses, social workers, and pharmacists
- Care management programs, such as Transitional Care Management
- Communication strategies that build professional relationships and improve quality
- Patient and caregiver education and engagement



