Value-Based Care | Patient Engagement
Maximizing the Value of Patient Assessments
Patient assessments are used in various settings by different medical professionals. They can be part of a proactive process (e.g., during an Annual Wellness Visit) or when some symptoms or signals indicate further assessment is necessary.
Not only can patient assessments reveal previously undiagnosed illnesses, but they also provide an opportunity for engagement and education to build healthier habits.
Let’s explore how care teams, particularly those within a care management or value-based care program, can maximize patient assessments.
What role do patient assessments serve?
Depending on the organization, patient assessments, including health risk assessments, can be conducted during inpatient hospital stays, before specific medical procedures, or as part of an annual physical or wellness visit.
They may also be used ad hoc during an in-person office appointment or a care management call if the patient mentions symptoms that merit further investigation.
The most common use of patient assessments is during the Annual Wellness Visit covered by Medicare for beneficiaries over 65. Specific assessments are required as part of the review.
While a physical is not conducted, a physician or other health care provider asks patients to complete a questionnaire called a health risk assessment. Through interview questions and evidence-based assessments, the Medicare Annual Wellness Visit can reveal previously undiagnosed conditions.
Additionally, by working together, the patient and provider can plan for near-term health goals and review what preventive care screenings, vaccines, and actions should be taken in the next 1-5 years.
Once complete, the patient should receive a Personalized Prevention Plan Services Report with a schedule of recommended tests, vaccinations, and screenings.
Benefits of integrating patient assessments into practice
Beyond being a requirement of Medicare Annual Wellness Visits, assessments can quickly evaluate whether a patient meets diagnostic guidelines or presents symptoms that require further investigation.
Additional benefits from using various patient assessments include:
- Discovering risks for specific conditions or issues, including genetic or lifestyle
- Addressing care gaps and quality care standards with individual patients
- Risk stratification for population health or chronic care program eligibility and enrollment
- Determining if the patient has unmet social needs that are creating barriers to healthcare service or treatment access
- Complying with regulatory and billing requirements
- Can generate additional reimbursement based on the assessment provided
Conducting patient assessments can lead to discussion about health goals and provide possible education opportunities.
Through evaluative conversations, the care team can build rapport and deepen the patient-provider relationship. This can lead to more active participation in care planning and commitment to treatment plan actions.
The most common types of patient assessments
A complete health risk assessment can cover numerous categories of topics, including:
- Medical history
- Hospitalizations and surgical history
- Providers and suppliers
- Medications and allergies
- Social history
- Mental health
- Lifestyle
- Functional status and support
- Home safety
- Life planning
- Preventive services
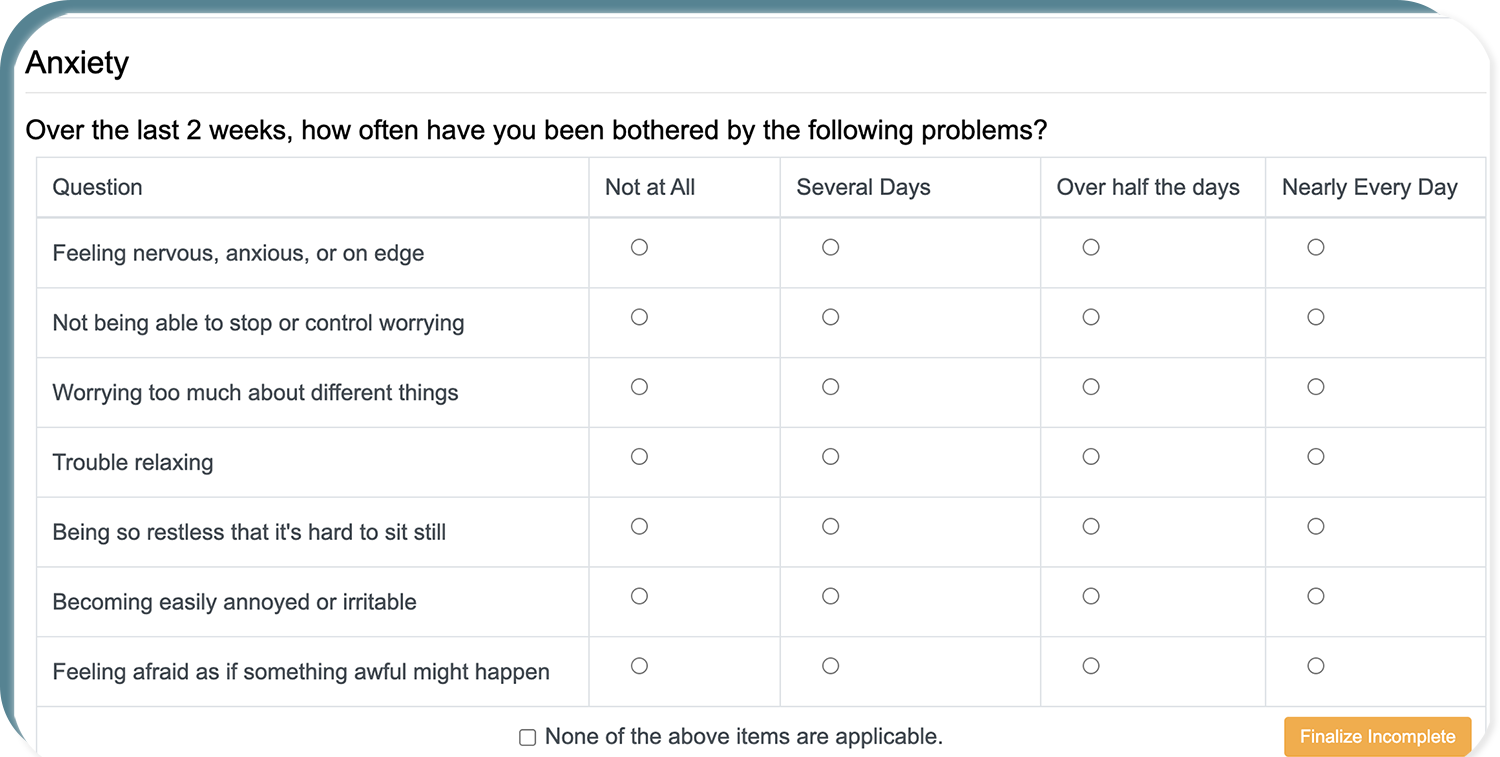
ThoroughCare supports the GAD-7 assessment (pictured) and several others.
For example, the ThoroughCare platform offers the following assessments as a sampling from the Annual Wellness Visit toolset. These are informed by recommendations from the American Academy of Family Physicians.
- CAGE (Cut, Annoyed, Guilty, and Eye) evaluates for substance dependency.
- DAST-10 (Drug Abuse Screening Test) provides a quantitative index of the degree of consequences related to drug abuse.
- MDQ (Mood Disorder Questionnaire) screens for Bipolar Spectrum Disorder.
- PAC (Post-acute care assessment) measures general functional status after an inpatient stay.
- PHQ-2 or PHQ-9 (Patient Health Questionnaire) inquires about the frequency of depressed mood and anhedonia over the past two weeks.
- GAD-7 (Generalized Anxiety Disorder Assessment) provides a seven-item instrument to measure the severity of generalized anxiety disorder symptoms over the past two weeks.
- The mini cognitive assessment tests memory and recall, using a three-word list of unrelated words and drawing a circle clock.
- An ADL (Activities of Daily Living) assessment measures a person’s functional status and ability to perform daily self-care activities independently.
Other assessments, like the Advance Care Planning module, guide the care team through conversations related to end-of-life planning.
Additionally, through a collaboration with Honor My Decisions, ThoroughCare offers Advance Care Planning education, decision support, and advance directive documents that are legally viable by state.
Patients can also create a video living will that can be viewed by designated family members.
Selecting patient assessments can be relatively easy—every medical specialty has recommendations on vetted tools. But it is paramount to ensure that assessments are seamlessly integrated with the care team’s workflow and enable data capture for future action.
Maximizing the value of patient assessments
Patient assessments are more than a checklist of questions.
When integrated with clinical workflow and tracked via technology and dashboards, they can provide a powerful way to monitor and resolve care gaps and support Chronic Care Management.
To select the best combination of process, platform, and assessment tools, consider these features:
- Ensure that assessment outcomes or scores are connected to widely accepted professional guidelines.
- Also, check to see that the results from assessment questions indicate recommendations and guidance for the next steps.
- Use the list above to vet any solution to confirm that it offers a comprehensive platform for wellness assessments.
- Automate eligibility checks to see if a patient should be enrolled in a value-based care management program.
- Determine if your team needs one-way or bi-directional interoperability with EHRs, health information exchanges, remote monitoring devices, advance care directives, or mobile apps.
- Look for tools that provide helpful dashboards, so the care team can visualize and interpret data through analytics.
- Investigate what risk stratification capabilities are available to use patient data for population health or care management enrollment.
Most importantly, keep technology in perspective.
Any platform should help the care team easily access trusted assessments, streamline data collection, provide risk scores, and facilitate appropriate action.
However, technology is a support and can’t replace the personal exchange between provider and patient. Avoid falling into a situation where the assessment is driven just by the tool and not the conversation.
Ultimately, patient assessments should strengthen and deepen each patient conversation. They should provide guidance and rigor to pursue better health and prevent future disease.



