Making Care Primary: CMS Now Accepting Applications
The Centers for Medicare & Medicaid Services (CMS) is accepting applications for its new advanced care model, Making Care Primary (MCP).
Set to start on July 1, 2024, this initiative will use gradual, population-based payments to support small, independent, and rural organizations as they transition to value-based care contracting.
The overall aim of the initiative is to reduce care costs and improve outcomes through more coordinated, whole-person care.
Making Care Primary eligibility
MCP is open to any Medicare-enrolled legal entity with a minimum of 125 attributed beneficiaries. At least 51% of a participating organization’s primary care sites must be within eight states—Colorado, Massachusetts, Minnesota, New Jersey, New Mexico, New York, North Carolina, and Washington.
These can include solo primary care practices, group practices, health systems, Federally Qualified Health Centers (FQHCs), eligible Indian Health Programs, and Critical Access Hospitals (CAHs).
Potential applicants can use the following summary of essential information from the Request For Application to aid in research and preparation for submission.
Launch timeline for Making Care Primary
Authorized as a primary care delivery and payment redesign model test under Section 1115A of the Social Security Act, MCP will be tested for 10.5 years from July 2024 to December 2034.
Performance year (PY) 1 will entail the program's first six months from 7/1/24 to 12/31/24.
Performance year 2 and forward will align with calendar years. Beginning January 1, 2025, PY2 will also be the first year when CMS provides performance quality and cost performance assessments.
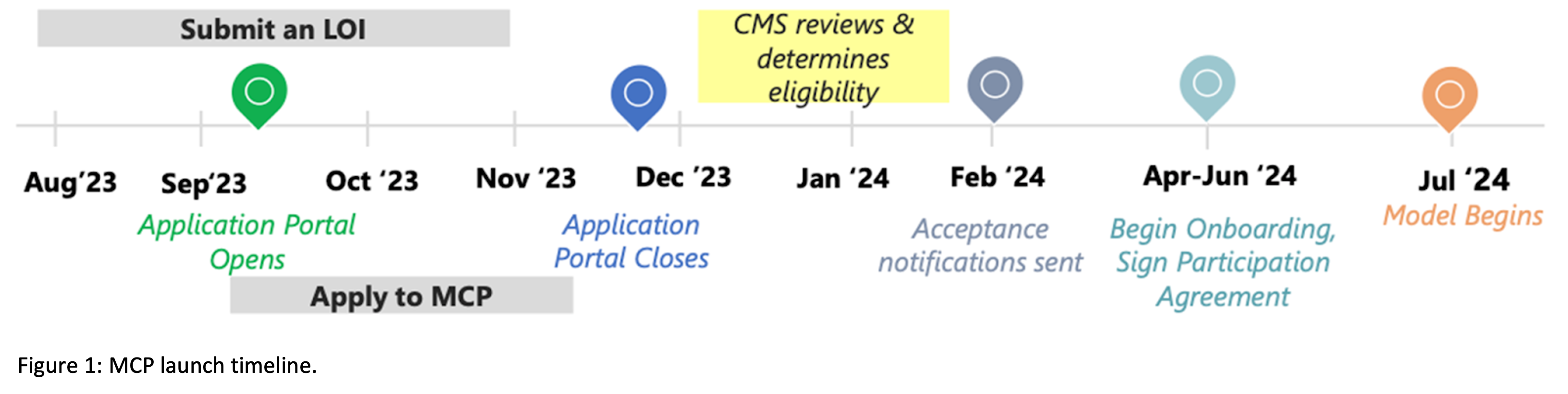
The MCP online application portal opened on September 5th and will close on November 30, 2023. Figure 1 shows the program launch timeline before the model begins in July 2024.
Making Care Primary design and payment model
MCP will take a three-track approach, summarized in Figure 2.
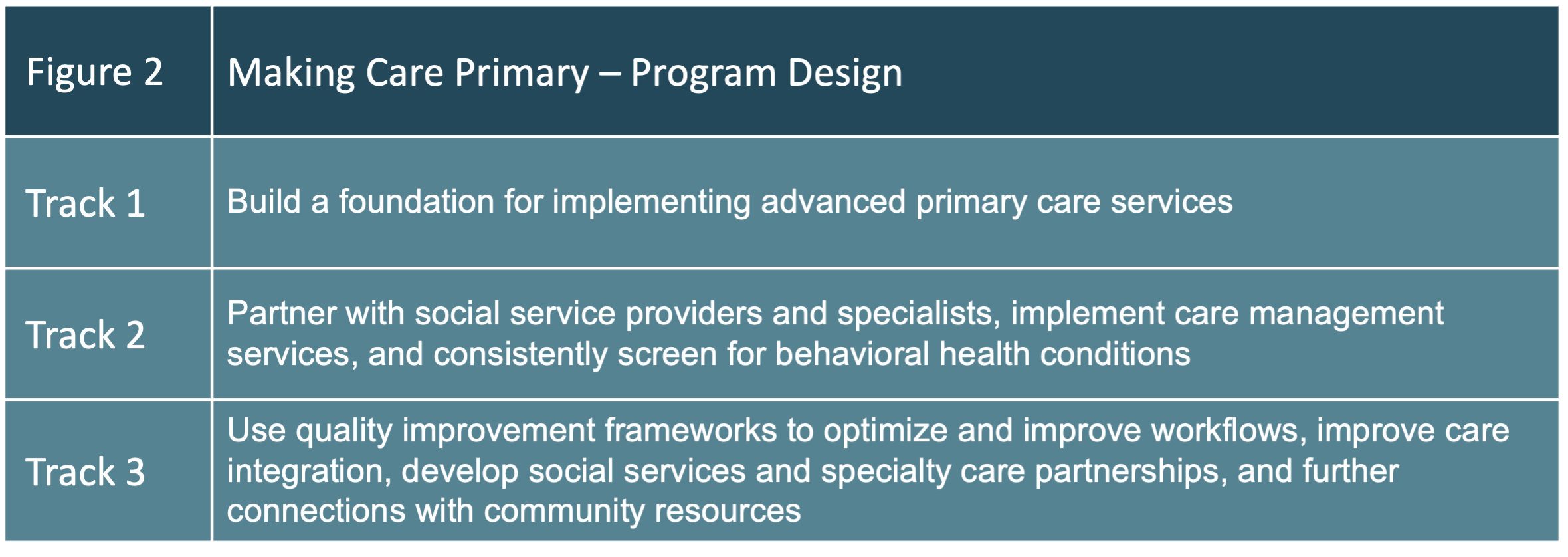
These three tracks provide a roadmap to increasing scope, capabilities, and financial payments.
A five-pronged care delivery design
MCP prioritizes several elements of care delivery, including:
- Care management
- Care integration with specialties like behavioral health, including collaborative care arrangements
- Community connections
- Health equity planning and data
The program aims to use evidence-based initiatives and lessons learned from past primary care model tests to support organizational and value-based care transformation.
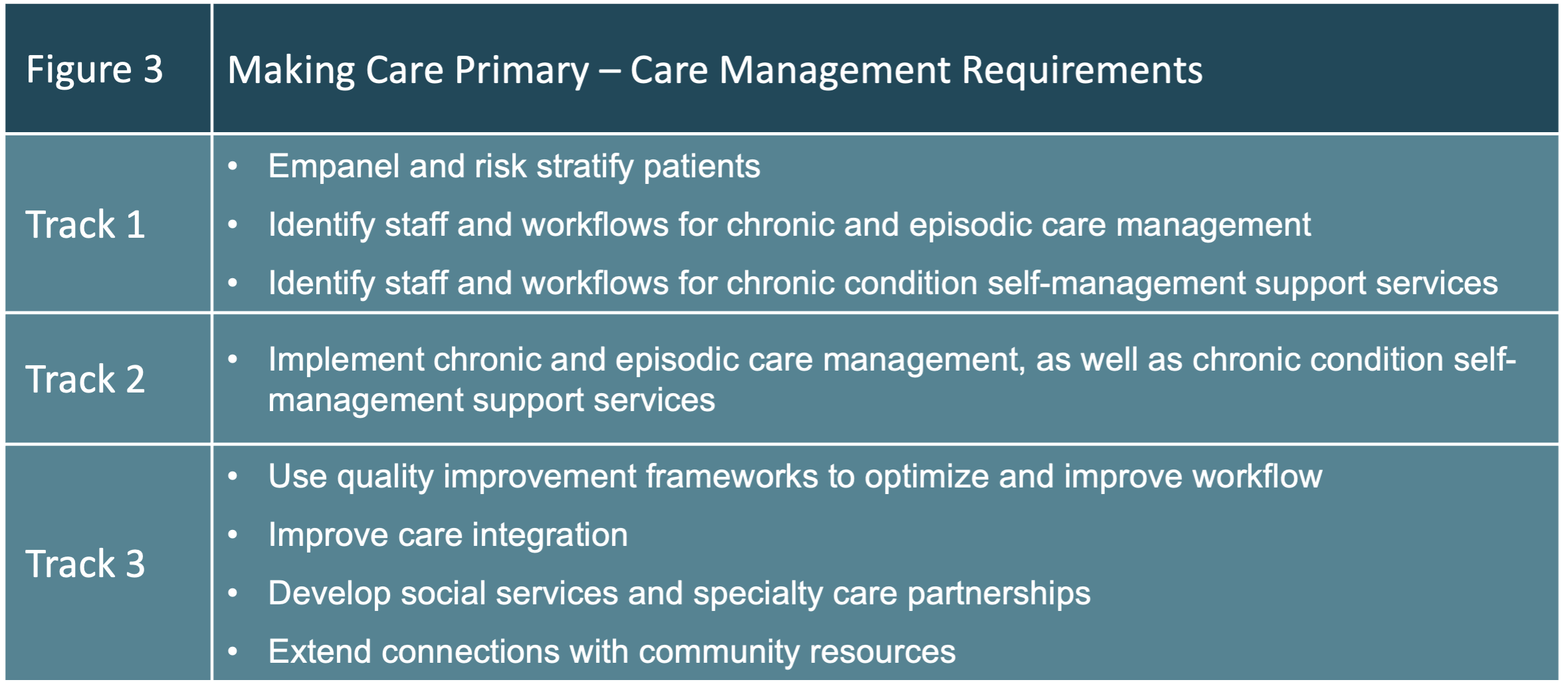
Care Management Domain
According to the Request For Application, “Participants will be required to build their care management and chronic condition self-management support services, placing an emphasis on preventing and managing chronic diseases such as diabetes and hypertension, and reducing unnecessary emergency department (ED) use and total cost of care.”
MCP participants are encouraged to create or increase their capacity and competency around delivering integrated, coordinated, and whole-person care.
Figure 3 highlights the overarching care management requirements.
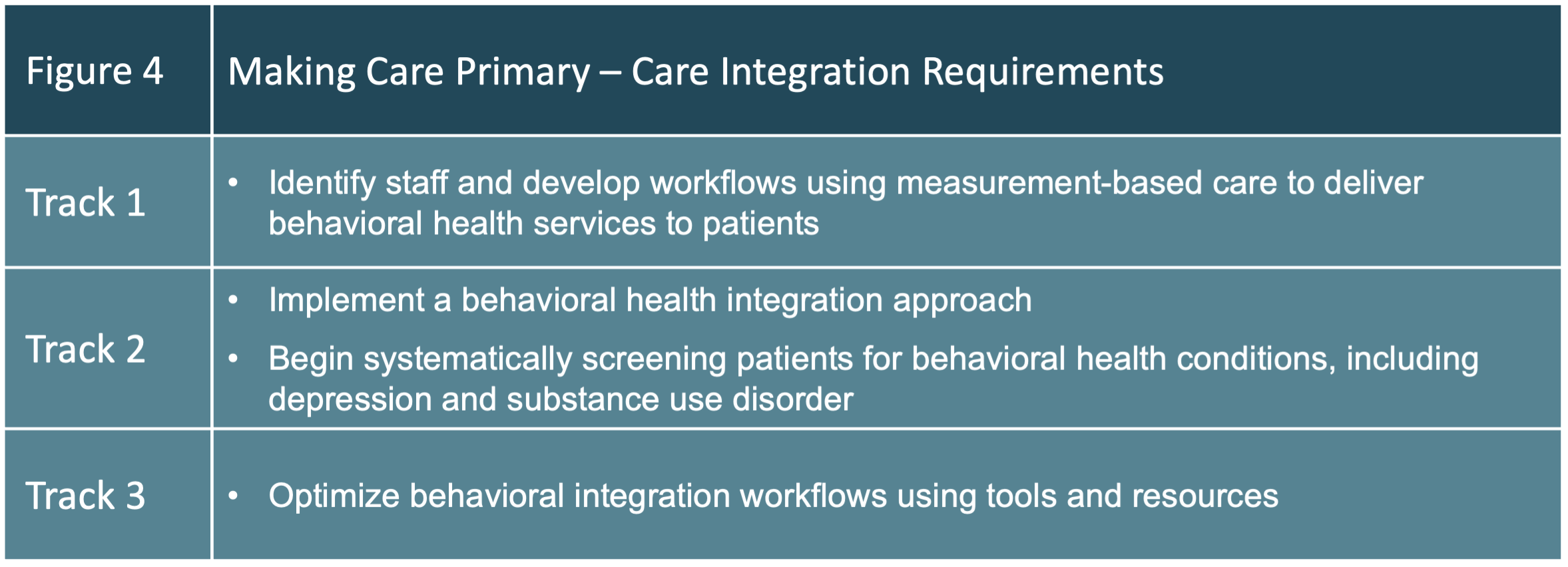
 Care Integration Domain
Care Integration Domain
MCP will require participants to strengthen their connections with specialty care, increasing behavioral health integration (BHI).
CMS sees BHI as an essential part of whole-person care that improves health outcomes and patient experience while reducing costs and treatment delays.
Figure 4 highlights the overarching care integration requirements.
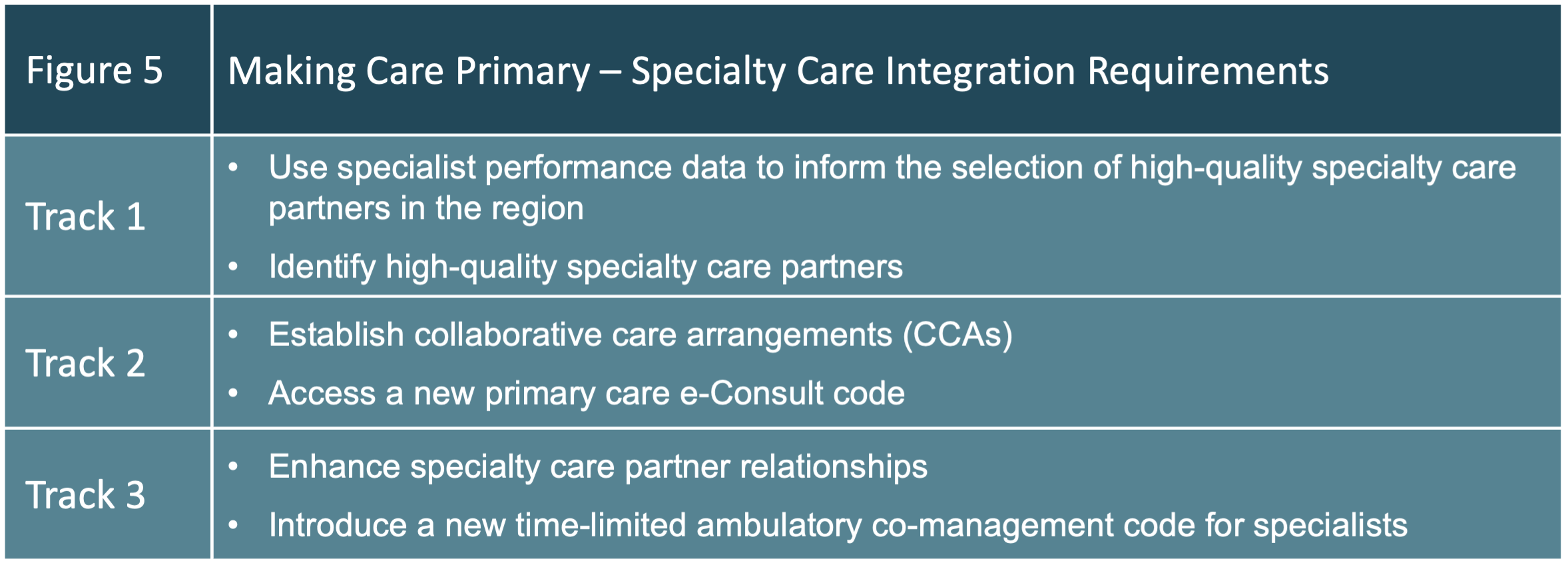
Specialty Care Integration
Facilitating coordinated partnerships between MCP primary care clinicians and high-quality specialists is an important goal. And, while beneficiaries can choose to receive services from any specialist based on coverage, MCP will provide payments, tools, and resources to promote high-quality specialty care integration.
Figure 5 highlights the overarching specialty care integration requirements.
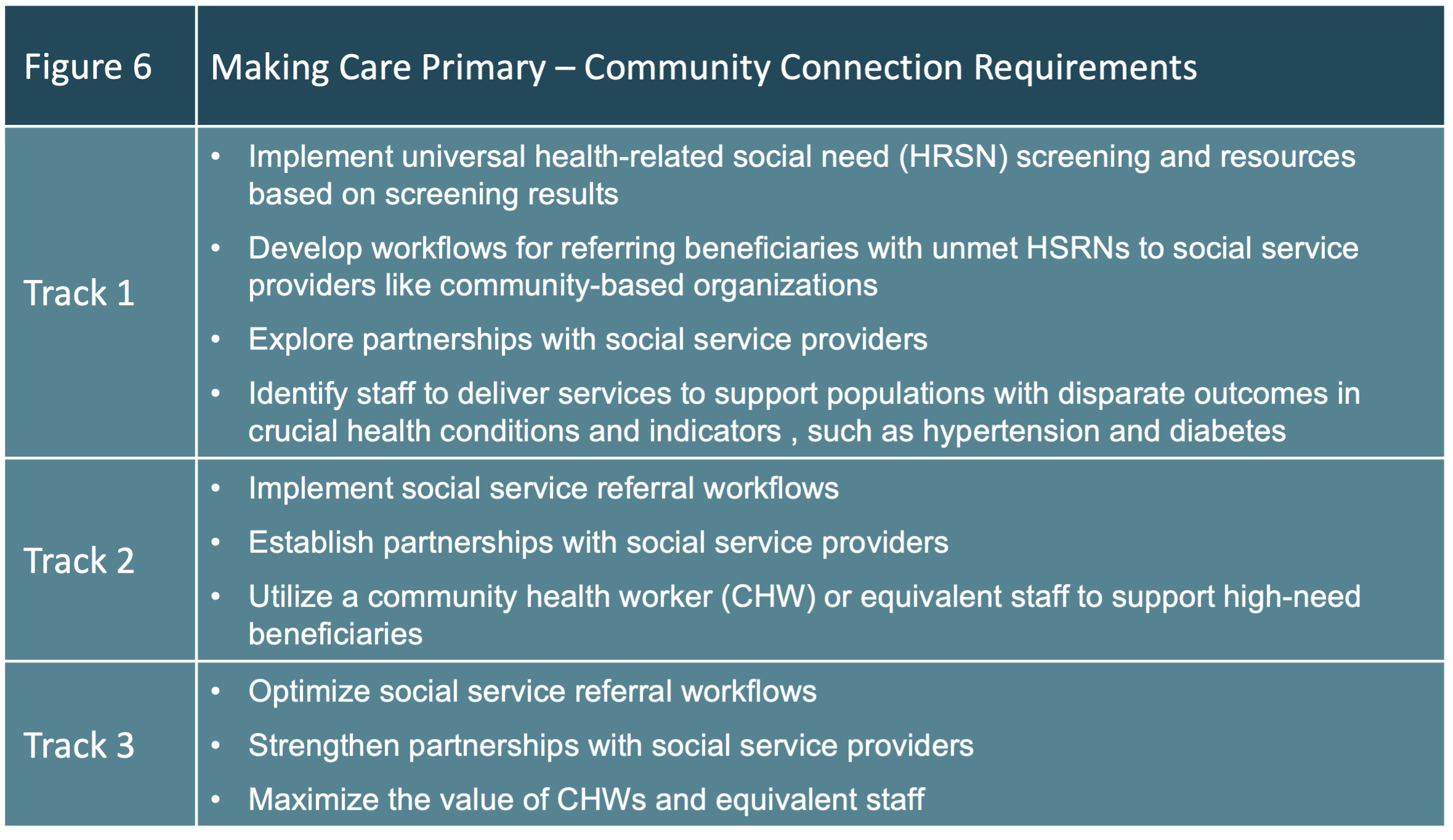
Community Connection Domain
To address health disparities and unmet social needs, MCP participants must identify health-related social needs in their populations and help patients navigate community support and services.
Additionally, community connection requirements will help participants meet health equity goals and may lead to reduced disparities among patient populations.
Figure 6 highlights the overarching community connection requirements.
Health Equity Plan and Data
CMS has prioritized health equity within the MCP initiative, in order to achieve high-quality care for Medicare beneficiaries.
MCP will adjust payments in light of clinical indicators and social risk levels and allow participants to reduce cost-sharing for beneficiaries in need.
Overarching participant requirements related to health equity include:
- Develop a health equity strategic plan that outlines how they will identify disparities and reduce them
- Outline steps to implement a health-related social needs screening and referral system
- Use of quality measures to assess the percentage of patients screened for social needs
- Collect specific demographic data and health-related social needs to evaluate health disparities in MCP communities
- Report on progress with the health equity plan to CMS annually
Making Care Primary payment design
CMS has created six payment types that support the initiative’s quality and cost goals.
Upfront Infrastructure Payment for Infrastructure Building: A time-limited, lump sum infrastructure payment for eligible Track 1 participants. This start-up financial support is for health IT investments, such as connecting with health information exchanges, e-consult technology investments, patient health data systems (i.e., patient portals), event notification systems, or EHR interfaces, which are not otherwise billable under Medicare FFS.
Enhanced Services Payment: A per beneficiary per month payment will be adjusted to reflect the attributed population’s risk level. Higher payments will be given to beneficiaries at the highest clinical and social risk levels. These payments, for participants of all Tracks, will be paid quarterly. They are intended to fund ongoing care management activities concerning MCP beneficiaries.
Prospective Primary Care Payment: A quarterly payment based on the historical primary care spending for each program participant’s attributed beneficiary population.
- Track 1: Continue to bill and receive payment from Medicare fee-for-service (FFS) as usual
- Track 2: Hybrid payments made, consisting of partial Prospective Primary Care Payment with reduced FFS payments
- Track 3: Full Prospective Primary Care Payment while certain FFS payments are no longer paid
Performance Incentive Payment: An opportunity for a positive adjustment to the sum of FFS amounts and Prospective Primary Care Payments. This will be based on the participant’s MCP Performance Measure Set.
MCP e-Consult: Track 2 participants are eligible to begin billing to a unique MCP e-consult code that continues for Track 3.
Ambulatory Co-Management: Specialty care partner physicians who work with participants in Track 3 will be eligible to bill a unique, short-term code focused on communication and collaboration.
Learn more about the specifics of each payment type in the Request for Applications.
Which Making Care Primary track is best?
The Request for Application provides a rubric, shown in Figure 7, for determining which Track could be a good fit for an organization.
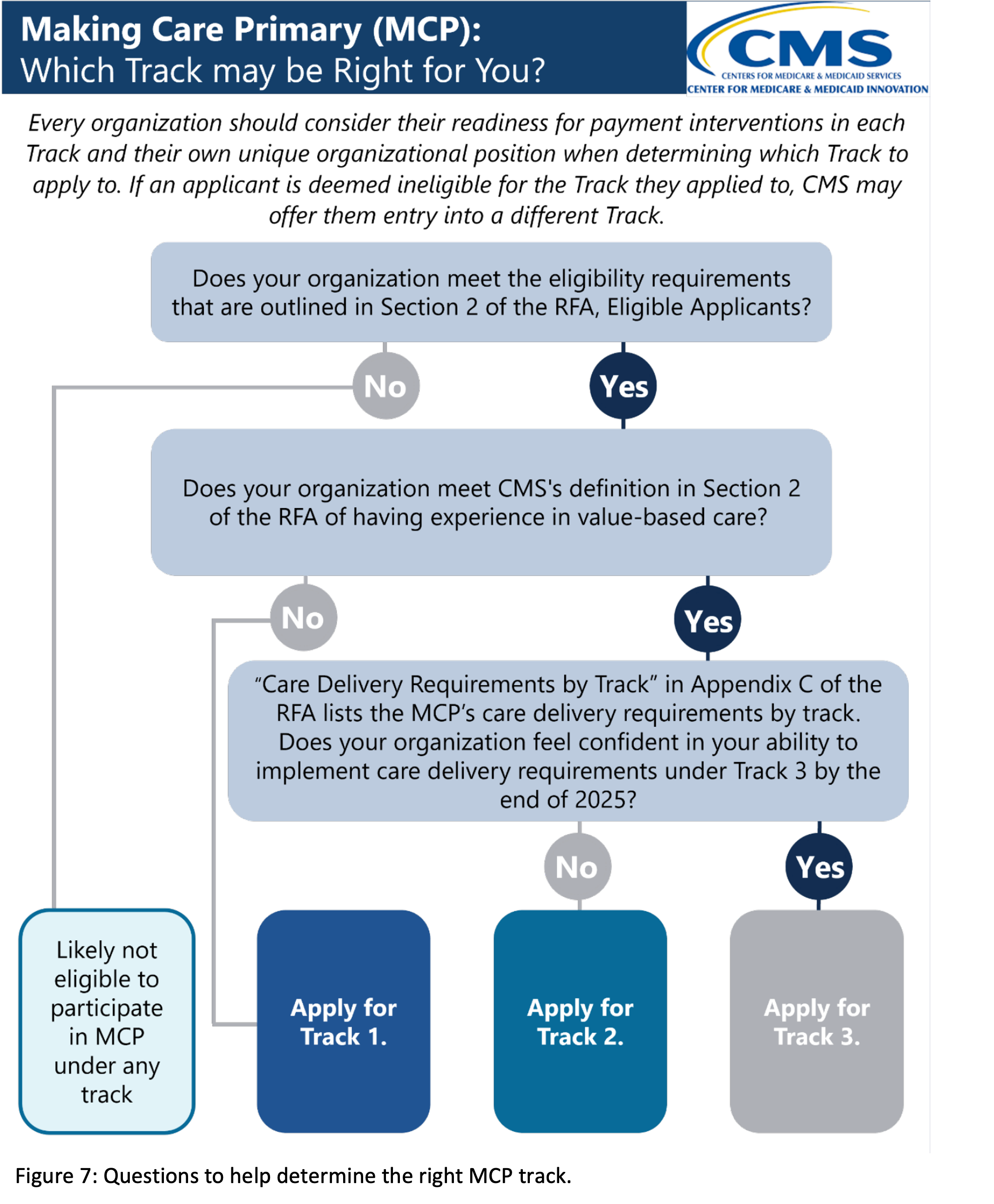
To be eligible for Track 1, applicants must have no value-based care experience, which CMS defines as having participated in performance-based Medicare initiatives, including:
- Primary Care First (PCF)
- Comprehensive Primary Care Plus (CPC+)
- Next Generation AGO (NGACO)
- Direct Contracting
- Accountable Care Organizations Realizing Equity Access and Community Health (ACO REACH)
- Medicare Shared Savings Program (SSP) ACO (having not deferred entry into a second agreement period under a two-sided model under § 425.200(e) in the five most recent performance years prior to the start of the agreement)
Track 2 and Track 3 can have previous experience with value-based care, but it’s not required. There are no additional eligibility requirements for Tracks 2 or 3 beyond those listed above for all applicants.
Next steps and resources
The first step would be to review the Request for Application, which includes detailed appendices and sample application questions.
Applicants are also encouraged to consider their readiness to carry out certain activities, including:
- Accept payment reforms described in the Payment Design section
- Assess performance measures described in the Performance Assessment section
- Meet the health IT requirements listed in Appendix B
- Meet the care delivery requirements of the desired Track as described in Appendix C by the end of 2025
- Sign the participation agreement
Note that MCP applications are not legally binding contracts.
If an applicant is eligible and accepted, they must sign a participation agreement with CMS before beginning participation in the model.
If an organization is interested but not ready to apply, CMS suggests submitting a short, online letter of interest. Other details, webinar slides, and contact information can be found on the CMS website.
How ThoroughCare can help
ThoroughCare provides the digital infrastructure for care management programs used by thousands of Medicare beneficiaries. With seamless EHR integration and data interoperability across health information exchanges and remote devices, our platform supports solutions for:
- Chronic disease management
- Remote patient monitoring
- Behavioral health services
- Wellness assessments
- Transitional care
Providers use ThoroughCare to seamlessly manage patient populations, create and maintain holistic patient records, motivate engagement, and visualize and interpret data to inform decision-makers.



