Remote Patient Monitoring (RPM)
How to Manage Diabetes with Remote Patient Monitoring
In the US, diabetes affects more than 38 million adults, making up 11.6% of the population, costing more than $306 billion in direct medical costs.
Adults aged 65 and older represent 29.2% of people diagnosed and undiagnosed with diabetes, increasing by 1.2 million each year. After adjusting for age and gender, people with diagnosed diabetes experience 2.6 times higher healthcare expenditures.
As the eighth leading cause of death in the US, diabetes is particularly pernicious. When left unchecked, the disease can create a cascading effect, causing or contributing to more than 57 other severe medical complications, including:
- Cardiovascular diseases such as heart attack and stroke
- Kidney failure
- Vision loss
- Erectile dysfunction
- Cataracts
- Non-alcoholic fatty liver disease
- Obesity
- Infectious diseases like tuberculosis
- Neurological illnesses like peripheral nerve damage, which can lead to amputation
As payor and provider organizations transition to more value-based arrangements and are held to greater diabetes screening quality measures, having more real-time and accurate patient data is critical.
Remote Patient Monitoring (RPM) is a game-changer. It makes diabetes manageable and helps individuals achieve better outcomes through accurate reporting, timely interventions, and enhanced patient self-management.
Benefits of managing diabetes with Remote Patient Monitoring
RPM uses a variety of Internet- or Bluetooth-enabled digital monitoring devices to gather clinical measures from patients at home, including:
- Glucometers
- Insulin delivery devices
- Blood pressure monitors
- Weight scales
- Pulse oximeters
- Thermometers
- Sleep and resting heart rate monitors
Remote Patient Monitoring for diabetes management has helped hospitals and accountable care organizations (ACOs) improve clinical outcomes. One study found that an RPM program for 2,000 diabetic patients improved a host of clinical, safety, and financial outcomes, including:
- 5% reduction in avoidable hospital admissions related to diabetic complications
- 25% reduction in ACO enrollees with an HbA1c of more than 9%
- 50% reduction in annual visits for diabetic patients
- Achieved an average PAM score above 80
- Achieved self-reported staff satisfaction with work above 80%
- Generated $500,000 in additional savings through reductions in avoidable ED and inpatient utilization
A survey of 25 provider organizations using RPM revealed that:
- 38% experienced reduced hospital admissions
- 25% reported decreasing readmissions and emergency department visits
- 17% realizing cost savings
The six core benefits of implementing a Remote Patient Monitoring program are at the heart of these outcomes.
More frequent, reliable, and accurate patient data
RPM devices can provide more frequent, reliable and accurate patient data. Care teams no longer rely on patients keeping glucose logbooks and bringing them to in-person appointments.
Additionally, access to continuous clinical metrics provides ongoing insights for physicians and patients. Everyone can learn from data trends, and patients can see the direct impact that diet, medication, and other lifestyle choices have on health.
Improve diabetes care plan adherence and address gaps in care
RPM supports diabetes care plan adherence by making ongoing monitoring more straightforward and more convenient. When coupled with insights and care team interventions, patients can gain more confidence and motivation when they see improvements and start to feel better.
Research has demonstrated how RPM can improve diabetes care plan adherence and mean blood glucose levels. One study found that more adherent patients increased engagement and transmissions by nearly 10%, from 82.8% to 91.1%.
Nonadherent patients improved their transmission rate by almost 15%, from 45.9% to 60.2%.
Faster interventions and better outcomes
Without RPM, patients and care teams might not realize concerning clinical trends before poor results manifest. With RPM, care teams can intervene and patients can take proactive steps to avoid exacerbations.
A meta-analysis found that RPM programs reduce HbA1c levels by 0.55 compared with traditional care approaches. One study of patients with type 2 diabetes using RPM for three months experienced improved outcomes, including:
- 67% of patients had a decrease in HbA1c
- 58% had a reduction in BMI
- 67% had an increased patient activation scores
Other studies found that an RPM-driven diabetes program significantly improved glycemic control of patients with diabetes after three months and six months compared to baseline.
Meet higher quality performance standards
RPM data also supports performance and quality reporting, which are vital in ensuring that diabetes care and outcomes meet clinical targets. For value-based care arrangements, RPM supports an organization’s ability to manage population health, particularly for costly conditions like diabetes.
Avoid chronic condition escalation or comorbidities
Patients with diabetes are at greater risk for a host of other conditions and comorbidities that can add complexity over time. Using RPM to collect timely data, coupled with data analytics and software, detects when patient results are out of bounds and alerts the care team to intervene.
Individual interventions can change the course of a patient’s health profile. And, when they participate in monitoring over time, they can avoid increased risk and new diagnoses.
Increase patient and provider satisfaction
RPM empowers physicians, care teams, and patients with timely data conveniently. Each can make decisions based on single readings or trends, saving patients travel, cost, and time, as well as saving providers from administrative and clinical inefficiencies.
ThoroughCare simplifies Remote Patient Monitoring
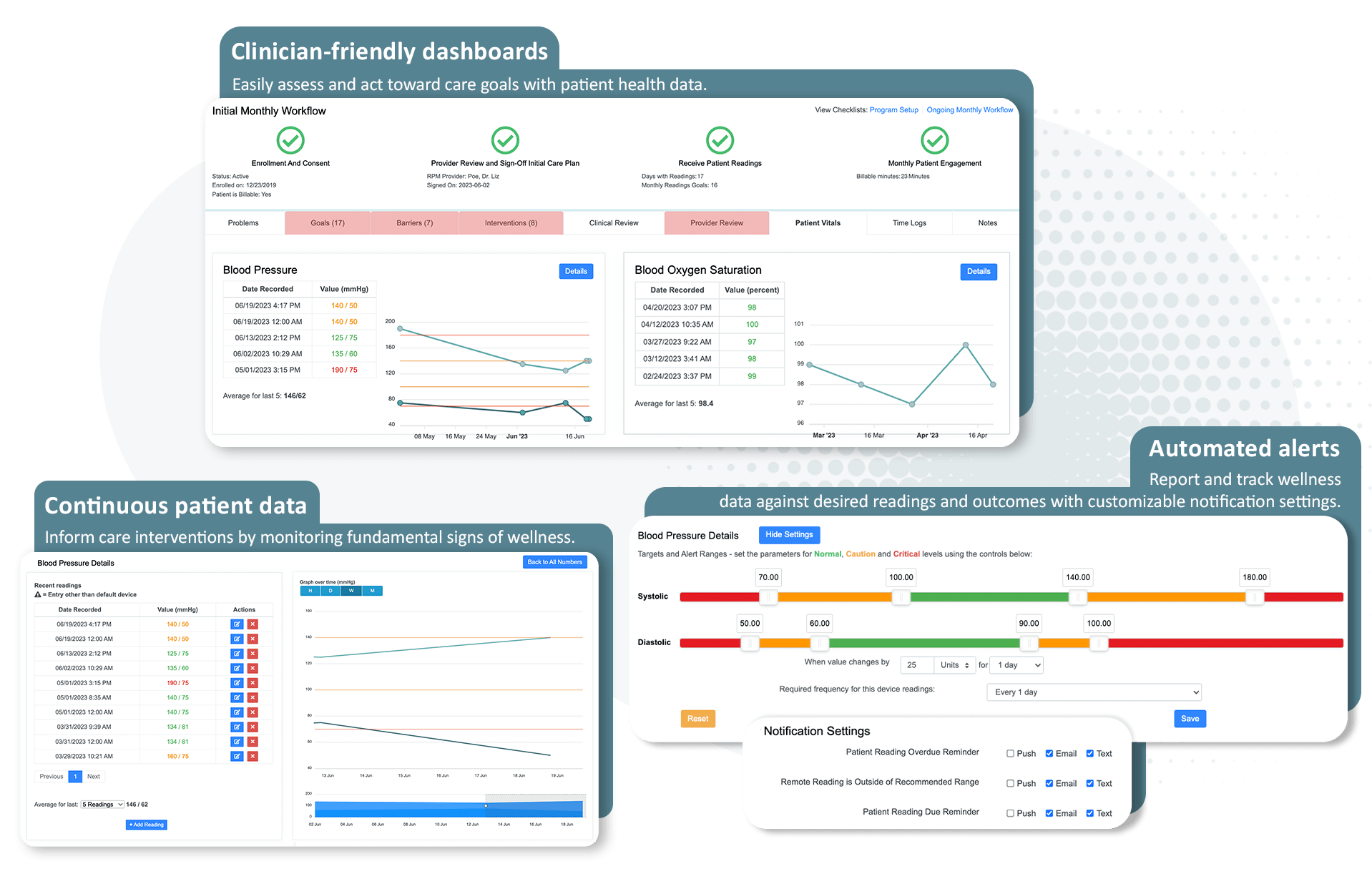
ThoroughCare’s care coordination platform simplifies and streamlines launching, managing, and scaling a Remote Patient Monitoring program. Built upon evidence-based workflows and data integration, our software empowers the care team, as well as billing and operations, to confidently take on an RPM service.
Real-time data and analytics: By leveraging RPM, healthcare providers gain real-time access to vital signs and health data, allowing for continuous monitoring of blood sugar levels without requiring patients to be physically present. Robust analytic dashboards and customizable reports support program oversight, population health management, and performance measure submissions.
Customizable RPM alerts and notifications: Enable early detection of potential issues as well as prompt interventions, leading to more effective diabetes management. Parameters, like blood glucose levels, can be set globally or individually to help assess, monitor, and manage gaps in care related to diabetes.
Directly order RPM devices: Devices can be ordered within ThoroughCare and shipped directly to the patient for added provider and patient convenience.
Seamless billing reports: ThoroughCare makes reimbursement preparation and submission easier with integrated RPM costs, CPT codes, and time logging.
Easily enroll and onboard patients: ThoroughCare has every care management program at the ready. Just input and enroll patients into the RPM program to activate that module in the software or work with our client success team to upload an entire diabetes patient cohort.
Maximize impact and revenue by combining RPM with Chronic Care Management
RPM can act as a standalone program, meeting all time, readings, and device requirements set by the Centers for Medicare & Medicaid Services (CMS). Providers can also maximize the value of RPM by adding additional programs, such as Principal Care Management (for one chronic condition) or Chronic Care Management (for two or more chronic conditions).
Create Diabetes care plans: Use evidence-based assessments to uncover barriers to care and create goal-oriented care plans. Engage patients with monthly touchpoints and educate them about their conditions with a comprehensive knowledge base of clinical content.
Care managers can also use the clinical content to feel confident when educating patients on managing diabetes.
Actionable analytics: Turn RPM and patient data into insights to identify and stratify diabetes populations and address gaps in care. These insights can be turned into tailored interventions and programs. Hone in on trends, patterns, and potential risk factors associated with diabetes. Utilize predictive models to anticipate possible complications or deterioration in a patient's condition.
Track care management touchpoints and tasks: Identify barriers to care plan success, like poor diet adherence or exercise intolerance, and implement appropriate goals and engagement.