What Are the 2022 CPT Codes for Remote Patient Monitoring?
Medical reimbursements are tied to Current Procedural Terminology (CPT) codes. They categorize and specify billing rates and rules for procedures, treatments, and care services.
If you’re a medical care provider, you likely know this. But do you know the rates and workflows for Medicare’s wellness programs? Like, Remote Patient Monitoring (RPM)?
Knowing the billing codes for RPM will give you a better idea of what’s expected, both by the patient and Medicare.
Understanding billing codes will also help you project revenues and optimize your staff’s capacity. Without this information, you risk disorganization and a clouded outlook.
At ThoroughCare, we’ve worked with more than 600 clinics and physician practices to help them streamline and capture Medicare reimbursements.
Our software assists with RPM’s rules and regulations, and it tracks all activities related to providing the program, such as patient vital collection, making it easier to bill for.
In this article, we’ll briefly review the requirements of RPM, as well as the program’s CPT codes. We’ll also provide an example return-on-investment (ROI) of an effective monitoring program.
With this information, you’ll better understand RPM billing expectations and standards. You’ll also see how care coordination software can simplify the program.
How Does Remote Patient Monitoring Work?
Medicare established Remote Patient Monitoring (RPM) as a general telehealth option for its insured population. Through various digital devices, doctors and healthcare groups can collect and analyze patient vitals on an ongoing basis, between regular office appointments.
Any patient covered by Medicare Part B can enroll in remote monitoring services. It pays for 80% of this benefit. Many secondary insurances will make up the difference.
RPM is a monthly billable program. Patients must receive at least 20 minutes of service each month for Medicare to offer reimbursement.
Reimbursement is also offered for setup and training related to RPM devices, as well as daily use by patients. We’ll cover this further below.
As the name suggests, services are delivered through remote interactions.
Patients take devices home with them, and they collect readings daily, which are then digitally transmitted to their provider. These readings can include, but are not limited to:
- Blood pressure
- Weight
- Blood glucose
- Heart rate
Data should be collected through a resource that is compliant with the Health Insurance Portability and Accountability Act (HIPAA), such as care management software.
Providers, on average, receive $52 for 20 minutes of service per month. Additional opportunities to meet higher billing thresholds are available, as we will detail below.
Providers may also receive an additional $56 per month when patients use their RPM devices daily.
How to Bill for Remote Patient Monitoring
There are five items required when submitting a claim through CMS:
- CPT Codes for each program you’re managing for the patient
- ICD-10 codes tied to each of the conditions you’re managing within that program
- Date of service
- Place of service
- Provider name
While it’s not needed, it is helpful to know the care manager assigned to a patient in case you’re ever audited: When billing, you’ll calculate the time spent with each of your patients monthly.
These are the four steps you’ll take when billing:
- Verify CMS requirements were met for each patient each month
- Submit claims to CMS monthly
- Send an invoice to patients receiving CCM services monthly
- Make sure there are no conflicting codes that have been billed
CPT Codes for Remote Patient Monitoring
For 2025 reimbursement information, click here.
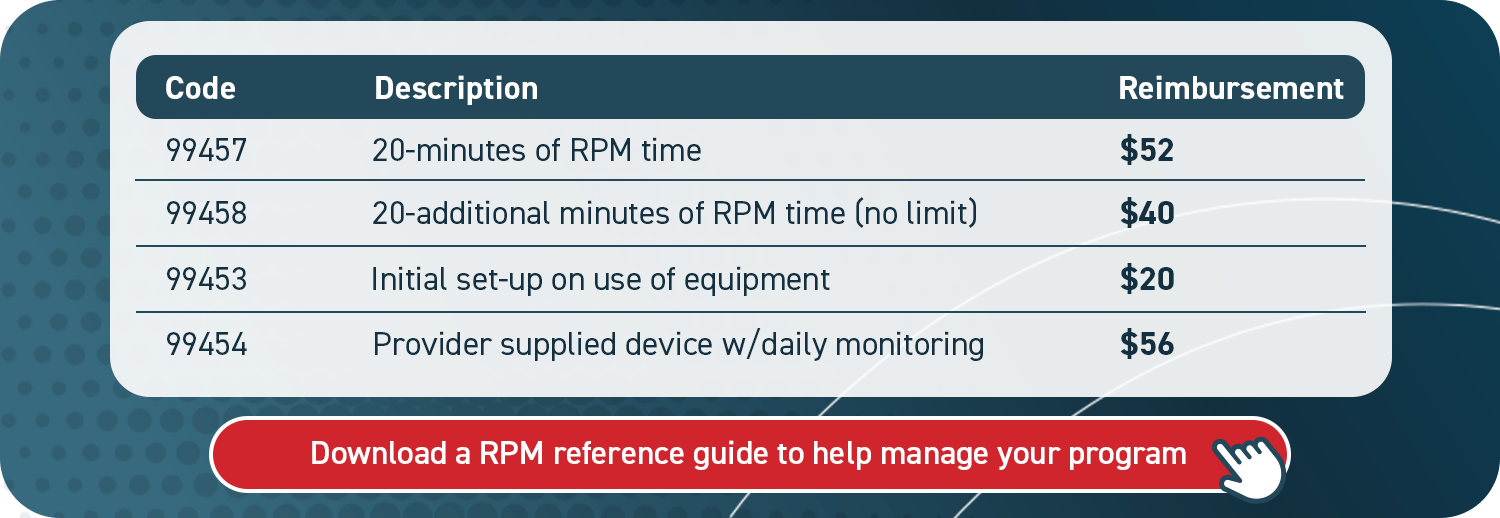
CPT codes for remote monitoring correspond to an exact activity, whether that be device setup or providing care services. The codes reflect different rates, each with its own restrictions.
Below, we break down the various types of billing codes for RPM.
For CPT code 99453, you may only bill it once per month, per device. For example, if you give a patient a blood pressure monitor and a digital scale in January, you can only bill 99453 for one of the devices in January. You’d have to wait until February to bill for the second device.
CPT code 99454 may only be billed once per month, no matter how many devices the patient is using. It should be billed on the last calendar day of the month only if the patient takes at least 16 daily device readings. A care coordination software solution can help you keep track of this requirement.
Remote Patient Monitoring for Rural Health Clinics
There’s confusion as to whether rural health clinics (RHCs) can offer RPM services. Medicare has, so far, excluded these organizations from the program.
The fact is, though, it is still possible for RHCs to provide RPM services.
They just cannot bill for RPM with the codes detailed above. They must utilize a more general CPT code, often applied to Chronic Care Management (CCM). This is CPT code G0511.
It pays approximately $76.94 per patient per month for 20 minutes of service. The code was created for “General Care Management,” and CMS has kept its definition very broad.
However, it cannot be used more than once a month per patient. So, if a patient participates in CCM, you cannot also bill G0511 for RPM usage. It’s one or the other.
What is the ROI of an RPM Program?
While the phrase return on investment (ROI) holds a financial connotation, a “return” isn’t entirely dependent on monetary value. General benefits are equally important, especially with regard to a person and their health.
Your patients will benefit from RPM because it places a preventive eye on their well-being while integrating the use of data. It also expands access to care without the burden of office visits.
Minimizing office or hospital time is a crucial point of value.
By allowing patients to stay at home, there’s less pressure on you and your staff, and there are more opportunities for high-risk patients to be seen. This leads to an overall improvement in the quality of care you and your practice provide.
As well, remote monitoring can help detect serious health issues before they occur.
Daily attention to a patient’s vitals can proactively address looming concerns, such as high blood pressure and its influence on a chronic or emergency condition.
On the provider side, both of these benefits play right to the goal of value-based healthcare.
Reduced hospital visits and improved care help satisfy certain performance indicators measured by Medicare. This can help providers sustain or improve their Merit-based Incentive Payment System (MIPS) score, which can raise reimbursement rates.
How Can Remote Patient Monitoring Produce Revenue?
As for RPM reimbursement rates, what is the revenue opportunity of the program?
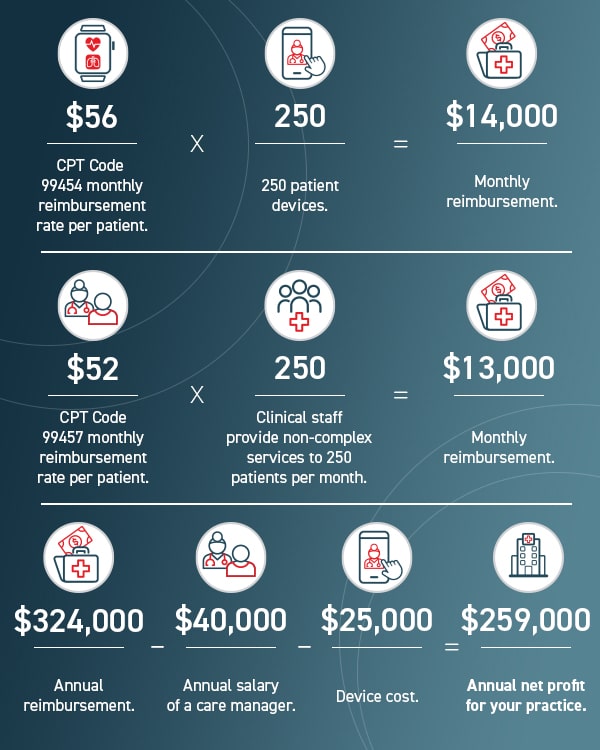
This figure does not include additional billable time beyond the 20-minute minimum. More time would produce a higher figure.
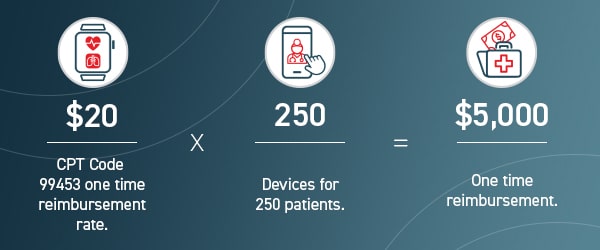
To help offset device cost, so long as you provide your patient with an RPM device, you can utilize a one-time CPT code designed for device reimbursement.
Offering an RPM program can generate revenue, as well as broaden care access for your patients and prevent emergency situations. The combination is inherently valuable.
Streamline RPM With Care Coordination Software
To deliver and document RPM services, you’ll want a system in place to manage your program.
A practical resource, such as care coordination software, will keep key details from being lost or overlooked. This will promote efficiency for you and your staff and help patients succeed. Care coordination software can streamline the collection of patient data, support staff workflows, and simplify billing. ThoroughCare’s software solution offers these exact features.
With a clinician’s eye, we’ve designed an intuitive platform that untangles the entire RPM process, so you and your patients can capitalize on it. Our care coordination software enables you to offer a whole suite of wellness services that pair well with RPM, such as Chronic Care Management (CCM) or Transitional Care Management (TCM).