Achieving Chronic Care Management Goals with Competitor Partnerships
Healthcare organizations continue to transition their approach to treating an aging population with a high rate of chronic illness. Payors and providers have ventured further into ambulatory settings where they can leverage more specialties, implement value-based care strategies, and launch tech-based programs, like chronic care management.
In this multifaceted landscape, however, how can one health system, health plan, or physician practice go it alone?
Sometimes, partnering with actual or potential competitors can help close care gaps, enhance access, improve health equity, and address social risks that threaten treatment and wellness. Thoughtful partnerships can help patients realize the benefits of chronic disease management.
When might partnering with a competitor make sense?
There could be many strategic and practical reasons to partner with a competitor.
Healthcare leaders may identify fragments in their patient care journey that they can’t cover adequately. They may have gaps in care due to a host of reasons, including:
- Geography and inadequate care access points
- Medical equipment or specialty care
- Specialized services, skills, or capabilities
- Programs, staff, or technologies used in chronic care management
Competitor organizations may provide some, or all of these.
Additionally, some practices or organizations may have long-standing relationships with the community, community-based organizations, and social services, making them uniquely suited to accelerate population or value-based objectives.
Some may offer an impressive track record in areas like disease or case management, population health, or data analytics that can add value to a new joint venture.
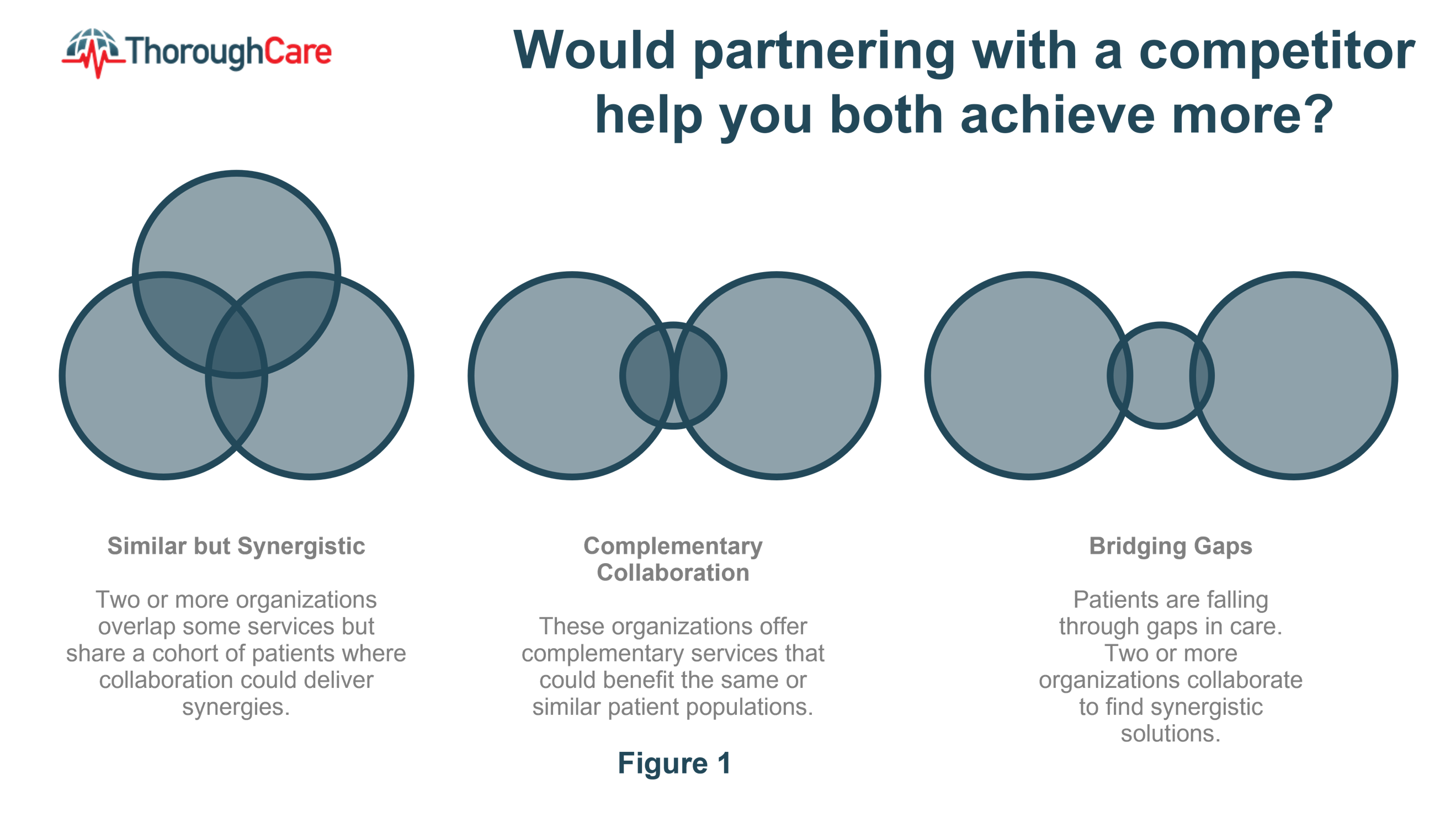
Figure 1 shows various scenarios where competitive healthcare organizations can work together to attain mutual goals.
Which types of competitors should be considered?
As healthcare organizations innovate to help patients achieve better outcomes, their focus tends to be on new services to increase capacity.
Health system vertical integration, through purchasing primary care practices and payvider arrangements, are possible strategies.
Another approach would be to look at other healthcare organizations whose current situations match the scenarios shown in Figure 1. From there, ask yourself whether you see potential partners that have common objectives. This could support the use of shared resources, capabilities, and technologies to achieve more.
Research from such an inter-professional collaboration between two competing health systems addressed fragmentation that occurred during care transitions for high-need, high-frequency patients. This collaboration led to a reduction in healthcare utilization and costs along with an increase in operating margin.
Health systems, hospitals with satellite clinics, Federally Qualified Health Centers (FQHCs), accountable care organizations (ACOs), retail stores, and retail pharmacies present possible partners.
Look for partnerships around chronic care management
Partnerships can flourish, even among traditional rivals, when there are common objectives that are high-risk or demanding.
Expanding or implementing a stand-alone chronic care management (CCM) program, or introducing CCM as part of a larger team- or value-based care model, requires a number of coordinated operational, staffing, and technology-enabled components.
When assessing or vetting potential partners for chronic care management, consider these questions:
- Do we have everything that we need to make our CCM program successful?
- Do we know how to handle CCM claims?
- For a VBC model, do we need other services or professionals to round out a complete care approach?
- How well do we know the CCM rules and requirements, and can we meet them?
- Do we have the right CCM management solution in place?
- What complementary services, tools, expertise, or data might our “competitors” have that we could partner to share?
If this is a new chronic care management program, review the typical elements used and assess how strong your organization is. Know where there are gaps that a partner could fill.
- Population identification: How will you identify which patients have one or more chronic conditions? What data patterns reveal where CCM could help these patients?
- Evidence-based clinical guidelines: Based on CCM patient data, how consistent is treatment implanted or adhered to by patients and providers? Where could CCM practices, communication, or follow-up tools support a more consistent treatment plan?
- Collaborative practices: What skillsets are available, and where could inter-professional collaboration or team-based care manage chronic disease better?
- Patient education and goal planning: Is patient education and coaching a strength? Are tools in place to establish SMART goals and track progress easily? Could partnering supplement the CCM program with additional support for medication adherence, behavioral health integration, home visits, 24-hour call centers, or appointment reminder systems?
- Quality measurement: How will you track process and clinical outcomes, patient satisfaction and engagement, as well as healthcare utilization, costs, and savings?
- Collaborative communication: If engaging internal teams or external partners, what is your plan for regular contact? What technologies will support treatment teams, patients, and program sponsors?
Creating a collaborative ecosystem for chronic care
Cross-organizational collaboration between hospitals or health systems might not be that radical, but building a collaboration ecosystem to address population health and chronic illness within a community could have a profound effect.
The potential becomes more evident as more payors enter the care delivery space.
Collaboration on a chronic care program could provide an opportunity to test working together before moving into a more formal partnership or joint venture.
In 2021, McKinsey looked into how health plans are redefining their role in care delivery.
Their analysis revealed that payors are using three approaches to pursue innovative managed-care models:
- Provider enablement via a management-services organization (MSO) or other services organization
- A platform-based ecosystem
- Direct ownership of care-delivery assets
This scenario could provide opportunities for health systems, physician practices, retail, and technology-based companies to create an ecosystem around chronic care management. This could be fundamentally aligned with value-based care, a bundled payment model, a Section 1115 waiver, or other alternative payment models.
The rapid acceleration of digital and technology-enabled tools has created an opening for competitors to come together and use solutions within a collaborative ecosystem.
Partnership starts with a conversation
Starting a successful chronic care partnership requires knowing your goals and your strengths while having an open approach to determine where there could be synergy.
Through shared resources, robust technologies, and clear roles and expectations, CCM partnerships hold promise to realize team-based, collaborative, and integrated value-based care.
How ThoroughCare Can Help
ThoroughCare’s intuitive platform can help healthcare collaborate and deliver digital care coordination, chronic care management, remote patient monitoring, and behavioral health integration. Our solution can help:
- Streamline the creation of patient care plans
- Support staff workflows with guided, validated assessments
- Help motivate patients through clinical recommendations
- Analyze patient risk factors and generate clinical recommendations
- Identify behavioral health conditions
- Track and log services for an audit-proof record of care
ThoroughCare supports comprehensive integration with leading EHRs, health information exchanges, remote devices, and advance care plans. We help healthcare visualize and interpret patient and operational data for actionable insight.



