Patient Engagement | Care Management
The Value and Process of Engaging Family in Care Management
More than 60% of older Americans receive help from unpaid caregivers; typically, these include family, friends, or neighbors. Engaging family as part of the patient’s overall care team has been shown to improve chronic disease management, including:
- Medication adherence
- Self-care
- Clinical outcomes
- Continuity of care
- Health literacy
- Readmission rates
- Emotional support and motivation
We’ll explore the benefits of engaging a patient’s inner circle in managing chronic illnesses through care management programs. We'll also highlight when and how to involve informal caregivers in patient care and how ThoroughCare facilitates deeper family engagement.
How is “family” defined?
It’s helpful to have a clear sense of what defines “family.” According to published research, the concept of family in healthcare has evolved to cover a more holistic perspective, entailing biological, social, psychological, and legal aspects.
In healthcare, a patient’s “family” can be defined as a social unit or collective whole formed by people united through genetic kinship, affinity, and emotional or legal relationships. The focus is on providing emotional, physical, or economic support rather than being limited to a biological connection.
According to CMS, the “term family is used broadly to include participants in a person’s healthcare, including informal caregivers, along with the primary caregivers of persons who are in need of the support of their caregivers to make informed healthcare decisions.”
When discussing family involvement in a patient’s care, it’s important to explore several questions with the patient, including:
- Is there someone who has either durable power of attorney or healthcare power of attorney?
- Who does the patient want to be the main point of contact and communication regarding their healthcare?
- Who does the patient trust most, and who wants to be involved in their care decisions?
- If needed, can someone come with the patient for in-person appointments?
- Who plays a role in the patient’s home, providing social support, in-person oversight, or assistance?
- Who is most accessible and capable of helping to facilitate communication and care, if needed?
While these questions are similar, they can uncover essential dynamics that make some members of the patient’s circle more appropriate. Ideally, as shown in Figure 1, the goal is to designate someone who can be a participatory member of the patient’s care team.

Figure 1: Spectrum of family involvement in decision making. Source: Abdul Rahman Jazieh, Susan Volker, Saadi Taher; Involving the Family in Patient Care: A Culturally Tailored Communication Model.
Research published in the Global Journal on Quality and Safety in Healthcare suggests that care teams identify the Most Responsible Family Member (MRFM) as part of a streamlined communication model, outlined in Figure 2.

Figure 2: Proposed communication model for engaging family. Source: Abdul Rahman Jazieh, Susan Volker, Saadi Taher; Involving the Family in Patient Care: A Culturally Tailored Communication Model.
The model suggests that this individual should have the following characteristics:
- The MRFM could differ from the next of kin or blood relative, but it should be appointed by the patient and willing to provide continuity of care.
- The MRFM should be identified to all care team members, including other family members.
- The care team must strive to have accurate and up-to-date contact information for the MRFM.
- The MRFM should be the first line of contact with the family if communication is required.
In addition to identifying the main point of contact (referred to in the research as the Most Responsible Family Member), the care team should determine whether communication with the family via the MRFM is mandatory or optional.
The research model suggests the following as mandatory points of contact:
- At the time of admission at the hospital
- During the discharge planning process and at the time of discharge
- Before any procedure (as part of consent) and updated after the procedure
- Any significant change in the patient's condition, particularly life-threatening situations
- When an advance directive needs to be exercised or Advance Care Plans accessed
- On request of the patient or other family members with the patient's approval
In addition to identifying the right person or people to join the patient’s circle of support, it’s helpful to determine the most critical times when family engagement should be initiated.
The connection between care management and family engagement
Published in the Nursing Reports Journal, “Family’s Contribution to Patient Safety” explains that while the Person- and Family-Centered Care model (PFCC) isn’t new, it’s fundamental to improving healthcare communication, patient satisfaction, and safety.
According to the Centers for Medicare & Medicaid Services (CMS), parent-family engagement aims to build strong and effective partnerships with families.
Their strategy summary states, “Person and family engagement goes beyond informed consent. It is about proactive communication and partnered decision-making between healthcare providers and patients, families, and caregivers.”
With a team-based, holistic approach to patient care, care management programs are well-suited for family engagement.
Engaging family through care management adds value for patients and providers
Research demonstrates that family engagement in patient care supports improved safety, clinical quality, continuity, and satisfaction across care channels—from inpatient to ambulatory care.
Four outcomes stand out as the most impactful from family engagement.
1. Medication adherence and chronic disease management
One study by Reisman et al. found that family involvement in caring for patients with chronic illnesses like diabetes and hypertension improved medication adherence and disease management. Patients with family support had better glycemic control and blood pressure levels than those without support.
Another study by Rosland et al. reported that family participation in chronic disease management programs improved self-care behaviors and clinical outcomes, including better control of blood glucose and cholesterol levels.
2. Improved communication and health literacy
A study published in the Journal of Health Communication emphasized the role of family in enhancing communication between patients and healthcare providers. It found that patients with family support had a better understanding of their health conditions and treatment plans, leading to more effective management of their illnesses.
Another study by Shen et al. highlighted that family involvement increased health literacy among patients, which improved their ability to follow treatment plans and make informed health decisions.
3. Reduced hospital readmissions
A meta-analysis showed that family involvement in discharge planning and post-discharge care significantly reduced the risk of hospital readmissions. A study by the University of Pittsburgh Medical Center revealed that involving unpaid caregivers in the patient discharge process results in a 25% decrease in readmission.
Families helped ensure that patients attended follow-up appointments and adhered to post-discharge instructions.
Research has found that elderly patients with family caregivers experience fewer hospital readmissions and emergency room visits, attributed to better continuity of care and support at home.
4. Enhanced emotional and psychological support
A study published in Psycho-Oncology demonstrated that family support was critical in improving the psychological well-being of patients undergoing cancer treatment. Patients with active family involvement reported lower levels of anxiety and depression.
Another found that family involvement in the care of patients with mental health disorders improved treatment adherence and reduced symptoms of anxiety and depression.
When is the right time to engage family in care management?
As a team-based and evidence-based approach to coordinated care, care management programs strive to provide patients with standardized services tailored to their preferences, goals, and social risks.
In addition to patient engagement, pursuing family participation can enable care management teams through outside support, personal information, and insight, as well as a strategic ally to help patients act on their treatment plans.
Each care management program offers unique moments when engaging families can further goals and add value to the care team.
Chronic Care Management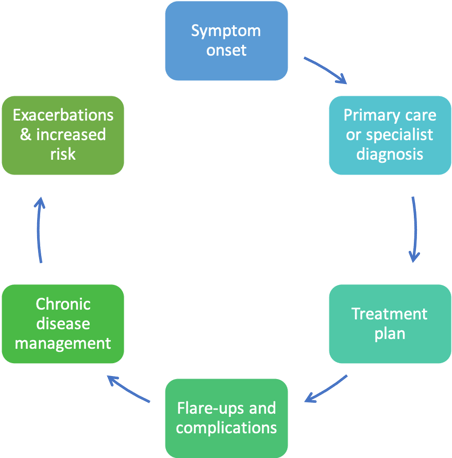
Figure 3 highlights the cyclical nature of chronic illness. While engaging family at the beginning is always helpful, it’s beneficial to identify and involve a family member when the treatment plan is first created and as exacerbations or inpatient admissions change the patient’s clinical risk status.
Early family participation can also help patients maintain a more positive attitude toward their treatment plan, motivating them to keep up with their monthly visits and care plan activities.
Transitional Care Management
After hospital discharge, about 50% of patients suffer from medical errors, and 19% to 23% suffer an adverse event with medication at the top of the list.
Numerous studies have examined the importance of the family’s role in preparing for and overseeing a safe discharge and transition after hospitalization.
Engaging key family members or informal caregivers who will support the patient at home is vital for safety, particularly in disease management where medication, nutritional, or physical regimens need to change.
The Medicare TCM program has structured requirements for the timeliness of follow-up, frequency of contact, and the type of oversight needed in the first 30 days post-discharge.
Advance Care Planning
Family engagement has been shown to ease difficult decisions. It’s never too early for patients to begin reflecting on their values and preferences. Ideally, Advance Care Planning should begin before a patient becomes seriously ill to ensure that their wishes are known and communicated.
Identifying and selecting a healthcare proxy with the patient is crucial to the ACP and advance directive process.
Some patients may wish to invite a trusted friend or family member to participate in the ACP process itself. When a proxy is chosen, documentation should be shared with them and others who may be involved should the patient require emergency or inpatient care.
Behavioral Health Integration
Research has shown that “family engagement in an older individual’s health care can help improve a patient’s mental health and motivation to continue with their course of care.”
For patients who have chronic behavioral conditions with additional physical illnesses, an integrated behavioral health care management program can be invaluable.
Family members complement the care management team, providing real-world insight, at-home support, and intervention guidance if needed.
Remote Patient Monitoring
Care management programs may also implement RPM devices to provide real-time clinical data, enhancing ongoing oversight of the patient’s condition at home.
Family can be helpful in the set-up and use of devices. Additionally, family can receive the same alerts that the care team does when readings are outside target measures or when the patient stops having readings.
RPM allows clinicians and informal caregivers to have concrete data to help avoid exacerbations and prompt interventions earlier.
How ThoroughCare facilitates family engagement in care management
Our platform engages the entire care team, as well as the patient and their family, when and how it is most helpful and appropriate. ThoroughCare makes care coordination and engagement easier by providing tools, data, and analytics as part of the workflow. That ease of integration is also true for patients and caregivers.
Through multimedia communication options, evidence-based education and assessments, and 24-7 resources, ThoroughCare supports shared decision-making, transparency, and timely communication. Here are a few features that highlight family involvement.
Identifying family: Across all of the care management programs offered through ThoroughCare, the care plan includes a resources and support section that asks two questions:
"Who is available in your support system to help you manage your health if needed?"
"Is your support system adequate and meeting your needs?"
This is typically where care managers, providers, or other care team members will indicate a person or people who are essential in the patient's healthcare.
Capturing family involvement: Our evidence-based health risk assessment, Annual Wellness Visit, and Transitional Care Management modules each include a section that asks if a caregiver completed the assessment on behalf of the patient. This is another way that ThoroughCare captures and engages family caregivers.
Remote notifications: Family members can also receive RPM notifications when their loved one’s readings are out of range, or the patient is not registering clinical readings, such as monitoring their weight or blood pressure remotely.
Sharing care plans and updates: Care teams can also involve family members via ThoroughCare by sending them CCM care plans and updates. They can also receive Advance Care Planning information and have 24-7 access to advance directive documents or media.
Offering field customization: ThoroughCare customers can tailor the platform’s custom fields and note boxes to document important family information, requests, and reference material.
Health education information integration: Our integration with Healthwise also provides access to evidence-based educational information on conditions and treatment, which can improve patient and family health literacy.
Key questions answered
How does engaging family in care management help patients and providers?
Engaging a patient’s family in their care management benefits both patients and providers in several ways. For patients, family involvement can improve adherence to treatment plans, as family members can offer support, remind them of appointments, and help manage medications. This support system can also reduce patient anxiety and improve overall well-being as patients feel more supported. For providers, involving the family can lead to better health outcomes and reduced hospital readmissions because family members can provide valuable insights into the patient’s health history and day-to-day behaviors. This holistic understanding allows providers to tailor care plans more effectively. Additionally, family involvement can enhance communication, ensuring that instructions and care plans are clearly understood and followed, ultimately leading to more efficient and effective healthcare delivery. Overall, engaging the patient’s family creates a collaborative care environment that promotes better health outcomes and provider satisfaction.
When is the best time to involve family in the patient’s care management?
The best time to involve family in a patient’s care management is as early as possible, ideally at the time of diagnosis or during the initial assessment. Early involvement allows the family to understand the patient’s condition, treatment options, and care needs from the beginning. This early engagement ensures that the family can provide informed support and participate in decision-making processes. Additionally, involving the family at the outset helps build a strong communication channel between healthcare providers, the patient, and the family, fostering trust and collaboration. It also allows the family to prepare for and adapt to the patient’s evolving care needs, ensuring a smoother transition through different stages of treatment. Early involvement is particularly crucial in managing chronic illnesses, post-operative care, and palliative care, where ongoing support and consistent care are essential for the patient’s well-being and recovery.



