How Rural Accountable Care Organizations Can Use Telehealth
Rural healthcare providers face unique challenges in providing care to the one in five Americans (67 million) who reside in rural, Tribal, or remote communities. The number of rural Accountable Care Organizations (ACOs) is growing to counteract hospital closures and buoy physicians experiencing lower reimbursement and greater responsibility.
ACOs have been shown to serve more patients with low incomes, disabilities, and members of racial and ethnic minorities. These communities experience chronic disease-related rates of death that are 38% higher for lower respiratory disease, 17% higher for heart disease, 15% higher for stroke, and 10% higher for cancer.
ACOs have demonstrated increased quality outcomes. These are associated with preventive care and show statistically significant improvements in diabetes, blood pressure control, breast and colorectal cancer screening, and other measures.
ACOs are also increasingly using funding from the Centers for Medicare and Medicaid Services (CMS) to implement technologies that support more accessible care.
These tools can enable better self-management and population health at scale.
Rural ACOs see 16% growth in 2024
ACOs participating in the Medicare Shared Savings Program (MSSP) have grown by 16% since 2024. This is despite ACO implementation being uneven between rural and urban areas.
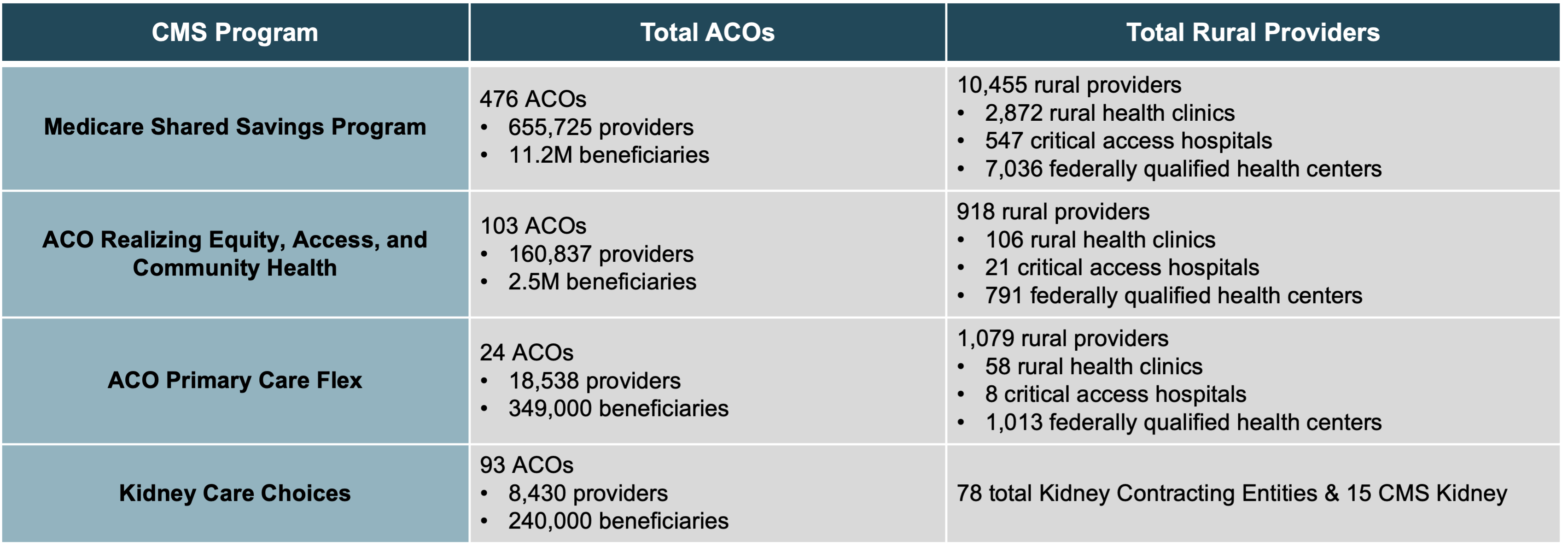
The table below provides an overview of the total number of ACOs in 2025 versus the total number of rural providers.
Because ACOs must have a minimum of 5,000 Medicare beneficiaries, many rural ACOs consist of numerous small practices to meet the covered lives requirement.
 Sources: CMS, American Hospital Association, Pennsylvania Office of Rural Health.
Sources: CMS, American Hospital Association, Pennsylvania Office of Rural Health.
New ACO program encourages rural participation with upfront payments
CMS has four active Accountable Care Organization payment programs, including MSSP, REACH, the new Primary Care Flex model, and Kidney Care Choices (KCC).
MSSP: The Medicare Shared Savings Program is a permanent program and the largest. In 2022, MSSP saved Medicare $1.8 billion and paid performance payments to 63% of participating ACOs.
REACH: Launched in 2023, the ACO Realizing Equity, Access, and Community Health model focuses on promoting health equity and access.
KCC: Kidney Care Choices (KCC) provides financial incentives for providers to manage care for Medicare beneficiaries with chronic kidney disease stages 4 and 5 and end-stage renal disease.
PC Flex: The ACO Primary Care Flex (PC Flex) model is the newest MSSP option launched in 2025 as a five-year voluntary model. Built on learnings from the ACO Investment Model (AIM), Flex aims to attract low-revenue ACOs that are typically physician-led and may include small or rural hospitals.
Flex consists of two new payments, including:
- The Advance Shared Savings Payment is a one-time $250,000 payment as an advance on shared savings
- A Prospective Primary Care Payment (PPCP) that is paid on a monthly basis
The prospective payment can help with staffing and technology investments that support a rural ACO’s launch or expansion.
Technologies rural ACOs can adopt to meet care challenges
Providers in rural areas encounter distinct challenges in delivering accessible, high-quality, effective care, especially for patients with chronic illnesses. These include:
- High fixed costs
- Relatively few patients
- Smaller operating margins
- Geographically distributed or remote patients
- Greater percentage of disabled or home-bound patients
- Limited local or regional specialists
Joining or forming an ACO can provide economies of scale, new funding sources, collaborative partnerships, and shared resources. When these ACOs implement certain technologies, they can leverage unique strengths and provide more effective long-term care to more patients.
While the technologies listed below have become commonplace in urban areas, they can have an outsized positive impact in rural communities. These tools can improve access, support ongoing oversight, care coordination, care management, self-management, and remote clinical monitoring.
Telehealth
Telehealth waivers granted during the COVID-19 pandemic will expire on March 31 and December 31, 2025, without congressional action.
The permanent adoption of telehealth policies in rural and connecting communities is critical to the many opportunities and benefits that remote communication offers providers and patients.
A research narrative review reported positive outcomes and experiences of telehealth use in rural populations, including:
- Acceptability and increased patient satisfaction
- Enhanced convenience and efficiency
- Decreased direct and indirect costs to the patient and provider
- Lower onsite healthcare resource utilization
- Improved physician recruitment and retention
- Improved access to care
- Increased education and training of patients and healthcare professionals
Research published by the National Rural Health Association recognized the instrumental role telehealth now plays in improving healthcare access. They found that telehealth saves $19 to $121 per telehealth visit by avoiding unnecessary emergency department visits.
Other research found that while urban use of telehealth decreased after the public health emergency ended, 29.5% of visits in rural areas continued to use telehealth. This equals 5.1% more than urban patients.
As outlined in Table 2, telehealth is a fundamental technology that significantly enhances access to local and regional providers, delivering services to more patients.
Through care coordination programs, telehealth provides a vehicle for communicating with and engaging patients regularly, connecting with specialists, and providing a host of educational and planning support.
Data analytics and interoperability
Data analytics and sharing can support more efficient and evidence-driven decisions.
Data sources can include an electronic health record (EHR), patient registry, health information exchange (HIE), regional health information organization (RHIO), or data aggregation software.
Figure 1, below, highlights the interplay between various ACO dimensions, including data analytics, interoperability, and other IT capabilities and outcomes related to the Quadruple Aim.
 Figure 1: Dimensions of digital health capability and their relationships to healthcare outcomes.
Figure 1: Dimensions of digital health capability and their relationships to healthcare outcomes.
Source: Woods, L., Eden, R., Macklin, S. et al. Strengthening rural healthcare outcomes through digital health: Qualitative multi-site case study. BMC Health Serv Res 24, 1096 (2024).
Data analytics not only provides insights that drive interventions, but it also supports the following:
- Collaboration with other providers and specialists
- Risk stratification for population health management
- Accurate risk-based coding
- Identify and fill quality care gaps
- Quality and compliance improvement projects
- Quality performance reporting
Armed with various data types and sources, rural ACOs can reap measurable rewards and improved outcomes from value-based arrangements.
Through in-depth interviews, the National Association of ACOs (NAACOS) revealed ACO leaders’ commitment to data analytics, saying “data drives transformation.”
Today, rural ACOs report using analytics to fine-tune risk stratification and care management approaches. Data helps ACOs know when to intervene with high-risk patients and avoid exacerbations.
Care coordination
A research study conducted in rural Missouri demonstrated how providers are using care coordination and formal care management programs to support patients. Some are also helping to address various social determinants of health (SDOH).
Researchers found a median care coordination population of 800 (range: 50–21,500) across a median of 11 case managers (range: 3–375).
Those providers reporting SDOH services were significant:
- 100% support transportation
- 86% support mental health
- 79% support food insecurity
- 71% aid housing
- 50% offer dental resources
Today, rural providers have access to numerous CMS programs for engaging in reimbursable care management.
Offering Chronic Care Management, for example, unleashes a set of evidence-based standards proven to deliver real-world impact.
Care management programs typically provide the following:
- Evidence-based patient assessments
- Care planning
- Motivational interviewing & goal setting
- Care coordination with other providers/services
- Self-management coaching
Other programs, such as Advance Care Planning and Annual Wellness Visits, complement chronic disease management. They help patients receive preventive care to avoid future diseases and tailor care based on personal values and clinical risk.
Remote Patient Monitoring (RPM)
As mobile broadband deployment expands in rural communities, providers can use Remote Patient Monitoring to extend patient oversight into the home or other facility.
Providers can collect data through RPM devices, such as weight scales, pulse oximeters, blood pressure devices, blood glucose monitors, and many others. They can then receive automated alerts when results fall outside desired parameters.
Research studies have found that RPM “offers a powerful tool for improving healthcare access and outcomes, especially for chronic conditions and rural maternal health, sustained investment in technology and infrastructure is critical.”
RPM pilots discovered that patients enrolled in the program pay greater attention to essential self-monitoring measures.
Access to real-time information enables patients to comprehend their health better. It allows both the patient and provider to make decisions collaboratively based on a collection of data instead of relying on just one in-office reading.
One rural program in Michigan demonstrated significant improvement in managing blood pressure and blood glucose. It achieved:
- An average reduction of systolic blood pressure of 27 mmHg
- A diastolic decrease of 11 mmHg
- A reduction in blood glucose readings of 25 mg/dL
Other programs have found value in focusing RPM on subpopulations of patients, providing targeted oversight. Rather than use RPM for all patients with heart failure, a study found that patients with mild depression, prior heart failure episodes, or an implanted defibrillator saw the most clinical improvement.
Artificial intelligence
Artificial Intelligence (AI) can help with population health management. This includes clinical decision and diagnostic support, data analytics, and care management automation.
By analyzing trends and predicting health risks, AI has shown promise for reducing healthcare disparities.
However, the greatest impact has been shown in automating evidence-based communications and care management tasks, such as AI-organized patient call summaries and next steps.
Pilots have found that AI support tools can increase care manager efficiency by 20-50%.
This can be particularly useful for rural ACOs that want to launch or expand care management programs with limited staff.
ThoroughCare enables care coordination for rural Accountable Care Organizations
ThoroughCare offers digital care coordination solutions and clinical advisory services to help ACOs achieve their goals. We ensure that leaders and care managers can access data that drives improved performance in clinical care, operations, finance, and compliance.
Our software offers functionality suited to the care management needs of ACOs, including:
- Performance metrics and cost reporting
- ACO oversight across members, including group functionality
- Medicare care management compliance and billing
- Timely interventions
- Personalized care plans
- Data integration and interoperability
Key questions answered
How has rural participation in Accountable Care Organizations changed?
While ACO implementation has been uneven and rural areas have lagged behind urban areas, rural ACOs have grown by 16% in the largest program, the Medicare Shared Savings Program (MSSP), since 2024.
For 2025, the four CMS ACO programs have nearly 700 accountable care organizations, including over 12,500 participating rural providers and caring for over 14.2 million beneficiaries.
The newest program, ACO Primary Care Flex (PC Flex), is the newest MSSP option, launched in 2025 as a five-year voluntary model. PC Flex aims to attract low-revenue ACOs, which are typically physician-led and may include small or rural hospitals. It also provides two types of payments: prospective and monthly.
Why are rural ACOs increasing technology adoption?
Technologies, including telehealth, data analytics, interoperability, care coordination software, remote patient monitoring, and artificial intelligence, are vital to helping rural ACOs meet their performance, clinical, and financial objectives. These tools optimize small clinical and care management staff to enhance healthcare access, ongoing monitoring, and patient oversight, as well as provide self-management support and goal planning.


.jpg)
