Healthcare Analytics | Data Integration & Interoperability
How Healthcare Analytics Are Used for Clinical Operations and Workflow
Data analytics is no longer a luxury for physician groups, at-risk provider organizations, care management service providers, home health agencies, and large health systems. It’s a clinical and business necessity.
The insights that data-driven decisions can yield are a must-have at a time when provider organizations are facing insurance market changes, value-based care, consumerization, increasing compliance requirements, and new provider market disrupters.
Data analytics enable proactive strategies for clinical and business objectives
Organizations can take a reactive approach to what patients, health plans, and government agencies bring to their door, or they can use data analytics to proactively strategize. Setting different priorities based on data can help maximize care quality, operational efficiency, and care team workflow to achieve clinical and business objectives.
As reimbursement, compliance, and value-based care models shift to paying physicians for taking care of populations of patients or managing high-need, high-cost patients, clinicians can tap into available data and analytical tools to better plan for staffing, interventions, and resources.
Data analytics adoption aligns with provider priorities
While data science, coupled with artificial intelligence (AI) and machine learning (ML) technologies, offer a host of analysis potential, provider organizations typically need more centrist capabilities. Taking a practical approach grounded in clinical, operational, or business objectives makes data analytics more accessible and useful.
According to the Brookings Institute, 44% of hospitals have developed a strategy for data governance or analytics. Other research shows that data analytics most impacts clinical workflow effectiveness and efficiency. Yet, there’s room for organizations to maximize the value of data analytics, considering that more than 30% are currently implementing a strategy to integrate data analytics into their clinical workflows, and 61% say they’re in the strategizing process.
A HIMSS Analytics survey revealed how healthcare organizations are most commonly using data analytics:
- 90% use analytics in clinical areas
- 85% use analytics in financial areas
- 77.3% use analytics in operational areas
For organizations that had not yet launched analytic capabilities but planned to do so, their objectives were clear:
- 59.1% will use analytics for the effectiveness of care and care quality measures
- 36.4% will use analytics for financial measures
- 31.8% will use analytics for population health and patient throughput
- 22.7% will use analytics for patient satisfaction
- 18.2% will use analytics for employee productivity
- 13.6% will use analytics for patient safety
- 9.1% will use analytics for chronic care management
The research shows that provider organizations are leveraging analytics aligning with their specific clinical, operational, or financial goals. This is a critical first step in choosing the right level of data science capabilities, data sources, and analytical solutions that meet unique patient populations and practice needs.
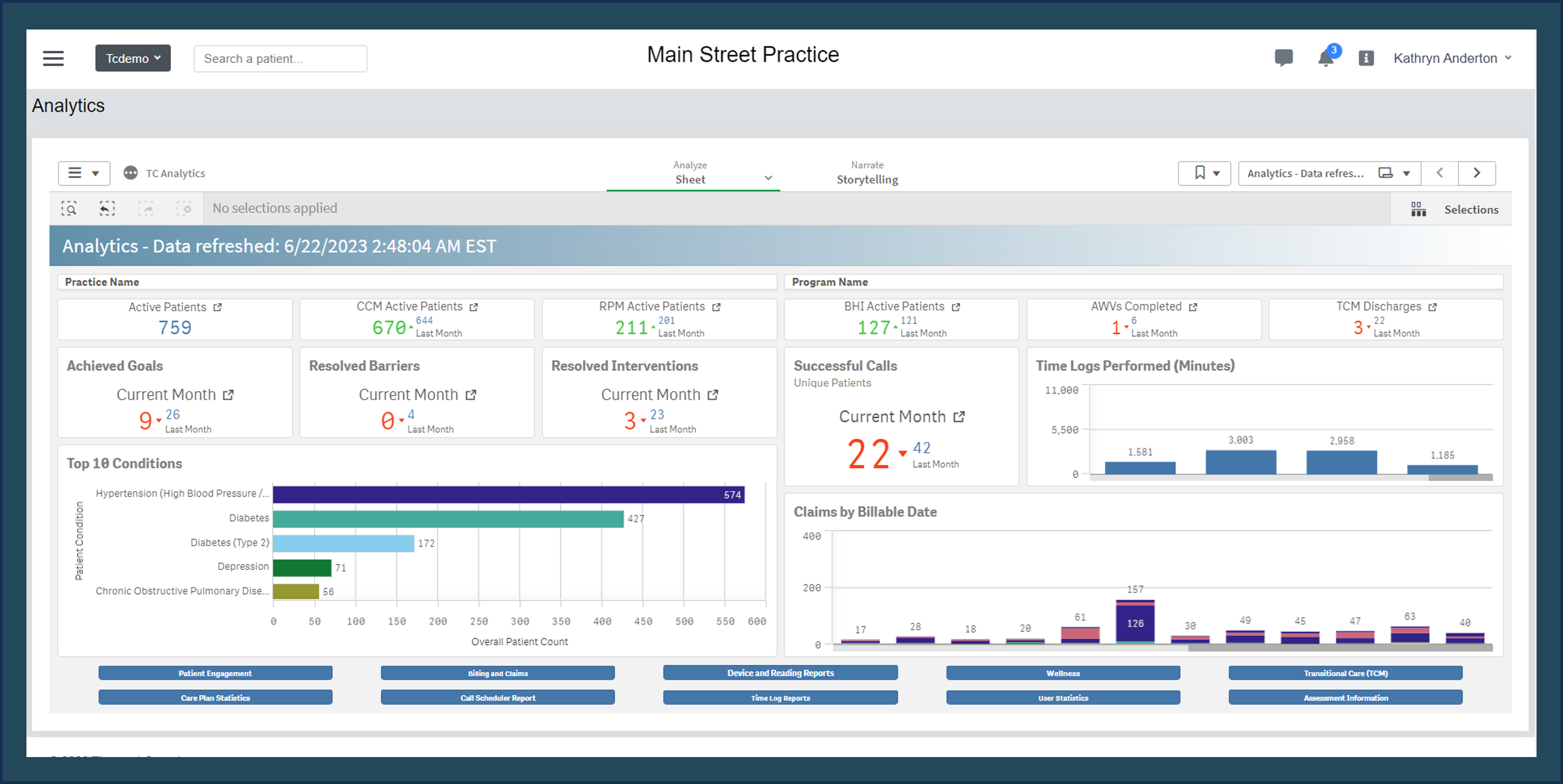
The ThoroughCare Analytics dashboard (above) provides an overall view of performance with key KPIs.
Discover unique provider- or practice-driven purposes for data analytics
Data, married with analytics, make a powerful tool to provide focus and clarity. However, maximizing the value from this pairing requires the right level of analytics sophistication, depending on the target use cases.
The overarching goal is to integrate information from various sources, generate meaningful, actionable insights, and prioritize decisions and actions that support them.
Choose the right use cases, data sources, and analytic types
Data-driven improvement requires understanding what problem data analytics should solve or what goal the analysis should support. Once a focus is established, analytics need the right data sources and clarity.
Healthcare data analysis use cases
HIMSS Analytics research highlights the top use case for healthcare data analytics:
- 58.1% use analytics for financial measures
- 56.8% use analytics for care quality measures
- 32.4% use analytics for patient safety
- 31.3% use analytics for patient throughput
- 28.4% use analytics for effectiveness of care
- 25.7% use analytics for patient satisfaction
- 21.6% use analytics for population health
- 20.3% use analytics for employee productivity
- 10.8% use analytics for chronic care management
- 6.8% use analytics for industry benchmarking
In general, data analytics use cases fall within four categories – clinical care; clinical workflow and operations; financial and claims; and compliance, regulatory, and legal. Here is a sampling of the types of use cases a provider organization may pursue when considering its strategic priorities in each area.
Clinical care data analytics use cases
As demonstrated, most use cases fall into clinical care quality, effectiveness, and outcomes.
But, even within this vast array of possibilities, a team, practice, or organization can’t tackle all clinically-related issues. Analysis may need to begin with a review of patient populations, reimbursement, business models, and quality compliance commitments to determine what further assessment and priorities merit attention. These could include:
- Insight into patients’ health-related habits
- Empower patients to embrace agency
- Engage, remind, educate
- Close gaps in care
- Population health management
- Chronic care management
- Identify or predict exacerbations, rising risk
- Diagnosis support
- Outcomes and utilization analysis
- Creating clinical pathways and standards of care
- Clinical quality performance
- Prioritize certain patients in need of proactive interventions
- Precision health for specialist care
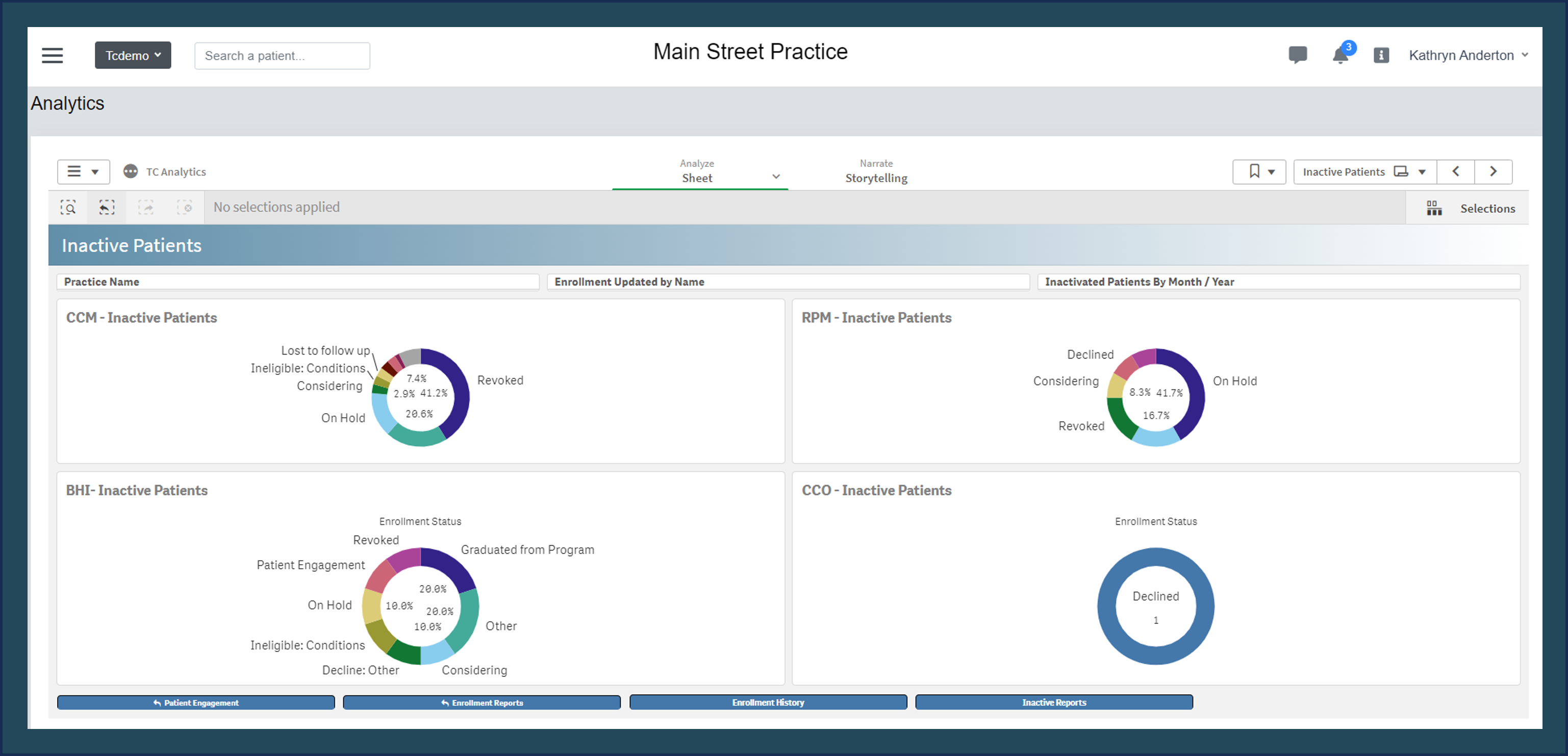
In ThoroughCare Analytics, the inactive patient dashboard provides reasons why patients are inactivated.
This can help provide understanding, so clinicians can address patient retention.
Clinical operations data analytics use cases
Operations analysis can span from front-office to in-clinic to back-office to reveal not only the current health of the organization, team, or practice but to establish where best to focus resources.
Use cases may determine how best to optimize the care team: who should do tasks to relieve physician or nurse administrative burdens?
The ultimate goal of clinical workflow reengineering is to ensure that each care team member can function at the maximum level of their license and qualifications.
- Forecast need and demand
- Enhance productivity
- Lean process improvement
- Reduce clinician burden
- Team-based care optimization
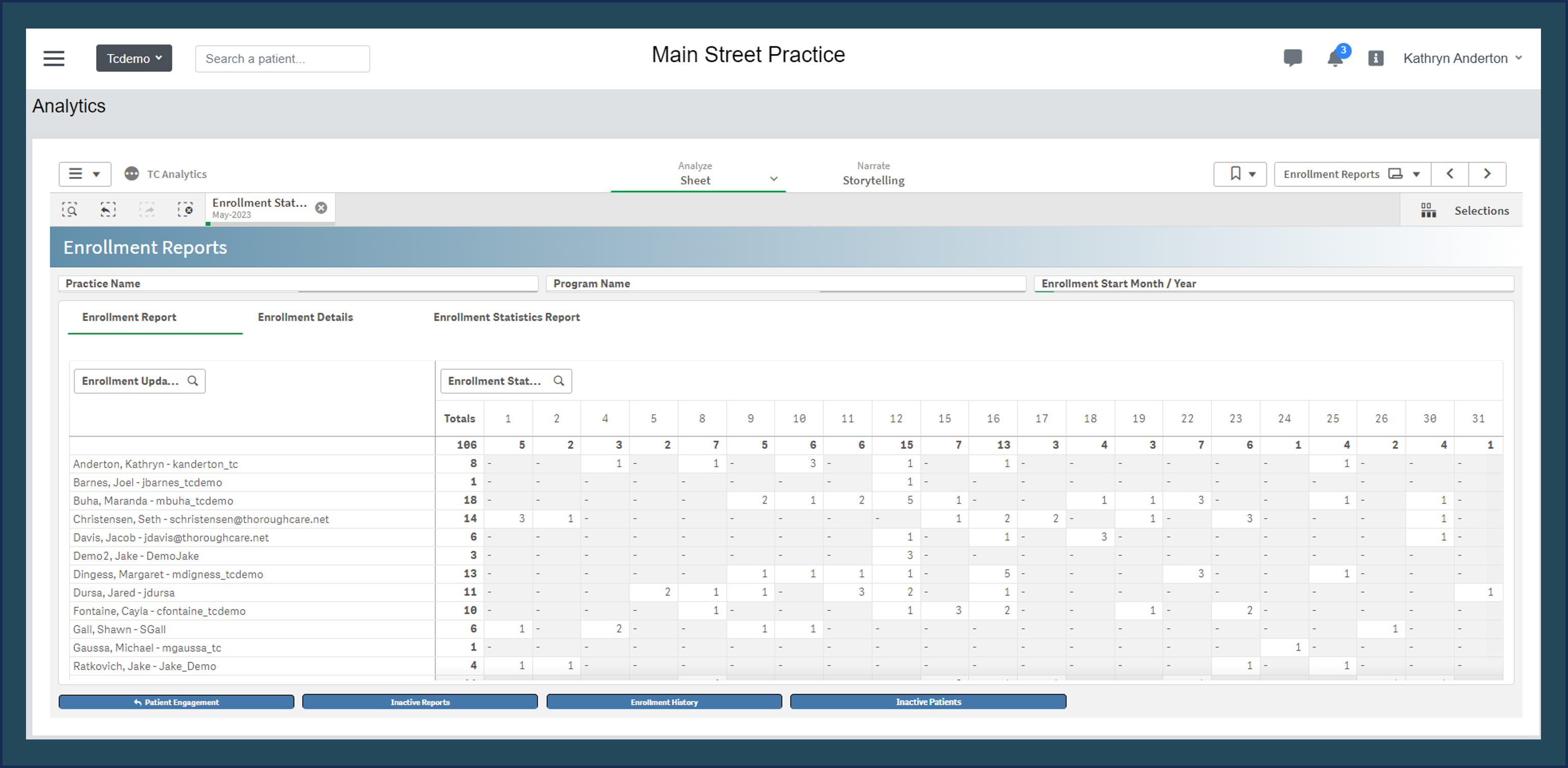
In ThoroughCare Analytics, the enrollment report provides an overview of new patients enrolled in specific programs.
It also breaks populations down by care manager to support operations and overall productivity.
Financial and claims data analytics use cases
Data analysis can answer questions like:
- “Should an organization or practice create an accountable care organization (ACO) or become a SNF-based provider?”
- “Would chronic care management or remote patient monitoring services enhance outcomes while growing the patient roster and contribute to revenue?”
- “Should we submit for an innovation grant or Medicaid waiver to provide care for specific patient populations?”
The answers to these questions can help:
- Reduce unnecessary spending
- Engage in value-based contracting and care, including ACOs and managed care organizations (MCOs)
- Inform payer contract negotiations
- Improve claims turnaround time
- Reduce denied claims
- Support business model decisions
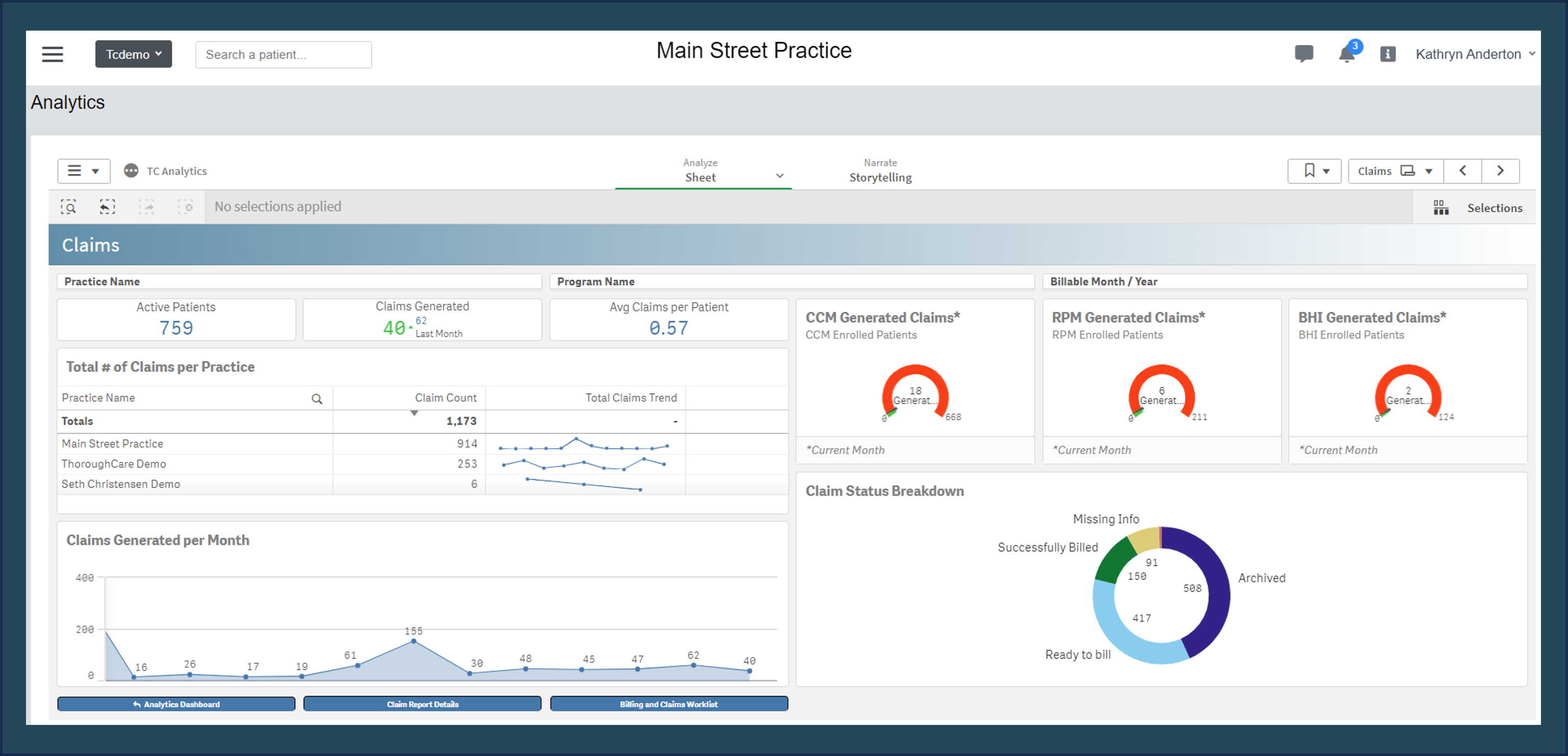
In ThoroughCare Analytics, the claims dashboard shows which programs and departments are generating more claims.
Compliance, regulatory, and legal data analytics use cases
Analysis that helps a provider improve quality care may meet higher levels of compliance that also yield more significant incentives and savings shared. Many of the prior use cases overlap with compliance and regulatory needs, and can support areas, including:
- Star Ratings
- HEDIS scores
- Accreditation and reaccreditation
- Quality measurement compliance
Four data analytic types
Figure 1 shows the four types of analytics and the question their analysis strives to answer.
Together, the four types are known as the Value Chain Model of Analytics.
Descriptive analytics can be used to determine how contagious a virus is by examining the rate of positive tests in a specific population over time.
Diagnostic analytics can be used to diagnose a patient with a particular illness or injury based on the symptoms they’re experiencing.
Predictive analytics can be used to forecast the spread of a seasonal disease by examining case data from previous years.
Prescriptive analytics can be used to assess a patient’s pre-existing conditions, determine their risk for developing future conditions, and implement specific preventative treatment plans with that risk in mind.
Data sources and types
Available data range from:
- Patient information included in an electronic health record (EHR)
- Claims and billing data from financial systems
- Care management information captured during chronic care coordination calls
- Population health management solutions
Analysis of EHR and claims data, which is easiest to access for most provider organizations, can be supplemented via integration and interoperability technology with data from health information exchanges (HIEs), patient registries and repositories, risk score indices, as well as patient-reported outcomes (PROs) and data from personal devices and remote patient monitoring.
Depending on the use case and the desired outcomes, easily-accessible data may suffice, or existing data may need enhanced data points. Advanced data science techniques, like predictive analytics, may necessitate additional types or sources of information.
Maximize the value of data analytics
The value of data analytics is quantifiable regardless of where an individual clinician, team, or program is on the data analytics journey. Rigorous measurement and data analysis is the lifeblood of modern healthcare decision-making and an essential part of improving patient care delivery, clinical workflow, and the financial health of an organization.
ThoroughCare’s shared technology platform enables integration with electronic health records, health information exchanges, remote monitoring devices, and advance care directives, supporting an inclusive view of patient data.
Data analytics reveal patient health trends and outcomes, facilitating more accurate risk assessment, cost management, and the promotion of evidence-based care practices.