The CMS Universal Foundation: Defining Care Quality
A March 2023 editorial in the New England Journal of Medicine spoke to the crossroads that the quality measurement movement faces.
The authors, who are leaders at the Centers for Medicare & Medicaid Services (CMS), spoke to a lack of alignment across their quality programs. This has created confusion and undue burdens on clinicians and health plans.
This lack of alignment has produced “tension between measuring all important aspects of quality and reducing measure proliferation.” This is despite CMS’s experience of administrating 20 quality programs and creating more transparent quality-performance information, better accountability, and focus on improving US healthcare.
CMS proposes the Universal Foundation
Announced through the NEJM perspective piece, CMS proposed a new building block approach to quality measures called Universal Foundation.
The new model focuses on quality measures that will create “more parsimonious sets of measures” to focus provider attention and drive quality improvement and care transformation.
This new foundation will apply to many CMS quality-rating and value-based care programs, such as Star Ratings, which payors now use to determine provider reimbursement in value-based contracts.
What are CMS’s goals for the Universal Foundation?
The new Universal Foundation will be critical to CMS realizing its National Quality Strategy, which centers on a person-centric approach throughout an individual’s life and the entire continuum of care, regardless of the care setting or payor type.
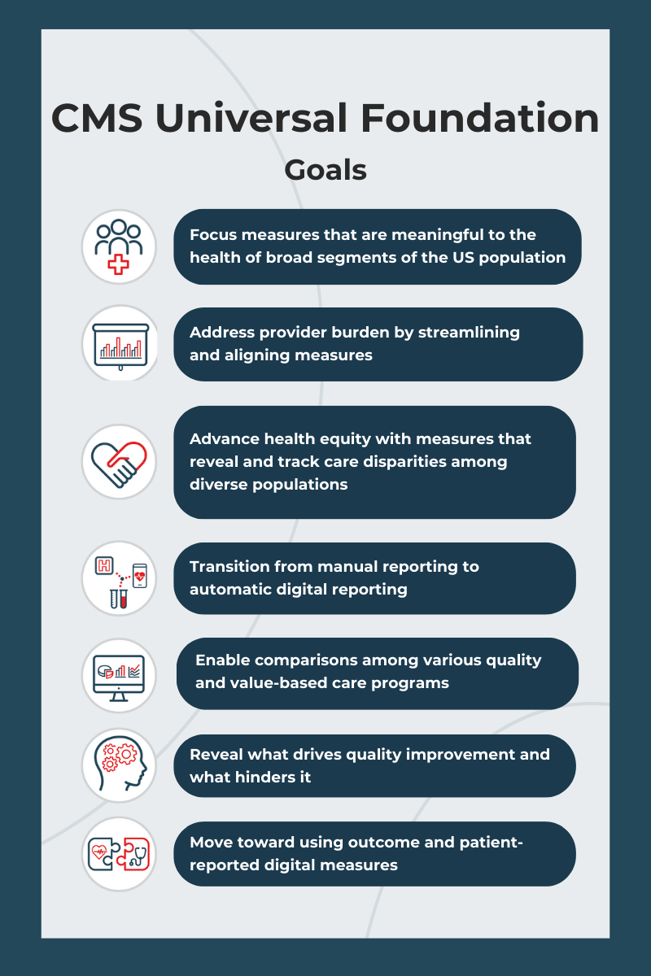
Through the Universal Foundation, CMS strives to achieve seven goals:
Ultimately, the Universal Foundation should follow a person’s lifelong healthcare journey, assessing quality from infancy to adulthood and during important health events like pregnancy, transitions through life phases, and end-of-life care.
Addressing quality measure burdens and confusion
In addition to these goals, the continual creation and development of quality measures has caused some counterproductive effects.
Health plan and provider leaders and clinicians are overwhelmed with performance reporting. Quality measures appear to be misaligned with typical clinical scenarios. Payors have also created their own quality measures, which adds to the confusion.
Providers and payors are unsure how to prioritize meaningful outcomes that align with national goals. Additionally, having multiple processes for selecting and approving measures has hindered the implementation of aligned measures. Lastly, this confusion has created a lack of consistency when value-based care incentives and rewards are designed.
The alignment between quality measures, performance priorities, and financial incentives is vital to streamlining focus and elevating national priorities. The Universal Foundation will support this by helping to identify CMS priority areas for measurement and revealing gaps where burdens and clarity are needed.
Prioritizing promising quality measures
The Universal Foundation’s quality measures align with many diseases and conditions responsible for the highest morbidity and mortality rates. These include diabetes, high blood pressure, and cancer.
CMS selected a set of preliminary adult and pediatric measures across six adult and four pediatric domains. It has prioritized the most promising measures to achieve national health and equity goals. It has also created a cross-center working group focused on coordination, development, and implementation of the aligned measures.
Health equity was of critical importance and was included as a measurement category domain. CMS aims to encourage the categorization of outcome data where disparities can be identified within populations.
Reception to the Universal Foundation
Reactions to the Universal Foundation have been mixed.
Some see it as a worthy goal to streamline and right size quality measures. The American Academy of Family Physicians (AAFP) shared its long-held stance against a “scattershot approach to quality measurement, which requires physicians to report on multiple sets of disparate performance quality measures across a wide array of private and public payers.”
AAFP’s Vice President of Practice Advancement, Karen Johnson, Ph.D., expressed that while well-intentioned, CMS’s efforts fall short.
“While we appreciate the intent of this announcement, focusing on a smaller number of existing measures that fail to recognize the value of primary care may be a viable interim step but should not deter us from pursuing long-term approaches that better reflect the holistic impact of primary care on outcomes that we care about — better health, smarter spending, and healthier people,” Dr. Johnson shared.
A recent article, related to primary care quality measures, cited a report created by The National Academies of Sciences, Engineering, and Medicine’s (NASEM) titled Implementing High-Quality Primary Care. In it, NASEM called for a “new ecology of primary care measures.”
Their report recommends:
- Measures for primary care must be parsimonious (meaningful and selective)
- Fit for purpose (aligned with stakeholder’s expectations)
- Allied with internal and external motivations (versus causing more physician burnout)
- Supportive of primary care value functions (leveraging trusting and therapeutic relationships)
While many will have opinions on what should and shouldn’t be included, the intent to develop universal measures is foundational to evolving care quality measurement and improvement.
Next steps at CMS
The CMS working group is moving forward with aligning measures while collecting feedback via listening sessions, requests for information, proposed rulemaking, and engagement with the medical community and general public.
In the meantime, the CMS Innovation Center will continue to test new quality measures based on a model’s quality aim. Since alignment is the primary objective, the Universal Foundation will be prioritized before adding new measures addressing similar quality aspects.
The Universal Foundation takes the first step to improving quality performance measurement
The Universal Foundation is CMS’s first step to simplify and streamline quality measures in alignment with national health priorities and strategies.
Their efforts could deliver a new era of quality improvement with far-reaching effects, helping provider and payor organizations achieve quality care with more consistent measures and less administrative burden.
How ThoroughCare Can Help
ThoroughCare can help health plans and providers track and report quality performance metrics across patient populations. With data analytics dashboards, healthcare organizations can:
- Monitor key performance metrics to spot gaps in care
- Interpret patient data as health trends take shape
- Close workflow gaps to further reduce cost
ThoroughCare enables decision-makers to act on data, align priorities at scale, and automate care plan suggestions to improve outcomes and engagement.