What’s in CMS’s 2022 Final Rule? (CCM, RPM, RTM)
In the final rule for its 2022 fee schedule, the Centers for Medicare and Medicaid Services (CMS) announced a key reimbursement rate increase for Chronic Care Management (CCM).
In addition, it has expanded coverage for Principal Care Management (PCM) with additional CPT codes. This and CCM’s rate increase will enable more providers to offer these services.
Other notable changes were made to additional Medicare programs. They’re also in the more than 2,400-page document. These include:
- An increase to CPT code G0511, which is used for general care management by rural health clinics (RHCs) and federally qualified health clinics (FQHCs)
- A slight rate decrease for Remote Patient Monitoring (RPM)
- The introduction of Remote Therapeutic Monitoring (RTM)
- The ability for RHCs and FQHCs to concurrently bill for CCM and Transitional Care Management (TCM)
These changes will affect you, your practice, and your patients.
So, here at ThoroughCare, we want to filter through the document and highlight the key changes that will matter to you and the programs we provide solutions for.
We’ve helped nearly 600 clinics and physician practices nationwide as they’ve transitioned to value-based care. We’ve made a point to stay informed and continuously tailor our software to simplify these programs.
In this article, we’ll cover the changes noted above. We’ll discuss how your practice can best leverage them to help increase revenue and improve care.
Rate Increases for Chronic Care Management
CCM now sports several higher reimbursement rates.
These come via the existing CPT codes you’ve likely become familiar with. The following chart details these higher rates and their associated billing codes versus the rates for 2021.
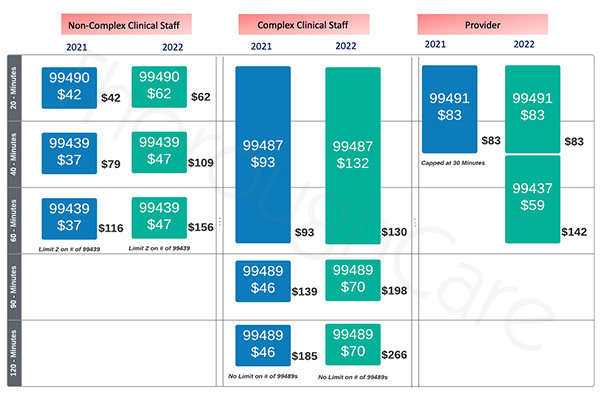 Please note: CPT code 99437 is a new CCM billing module. It is meant to allow providers who directly administer their CCM programs to bill for up to 60 minutes of time. Previously, providers could only be compensated for 30 minutes.
Please note: CPT code 99437 is a new CCM billing module. It is meant to allow providers who directly administer their CCM programs to bill for up to 60 minutes of time. Previously, providers could only be compensated for 30 minutes.
Looking ahead to 2022, it would make sense to focus your practice toward CCM enrollment. CMS is creating ample opportunities for providers to develop and scale this effective program.
According to the Journal of General Internal Medicine, patients reported several benefits with CCM. It improved access to their primary care team and strengthened care coordination.
This generally reduces the need for emergency room visits. According to Medicare, CCM can save on healthcare costs of up to $74 per patient, per month.
Expanded Billing Codes for Principal Care Management
PCM, which allows for the designated care of one high-risk condition, now accommodates up to 60 minutes of billable time, by both clinical staff and providers.
The following chart details the new rates and codes versus their 2021 counterparts.
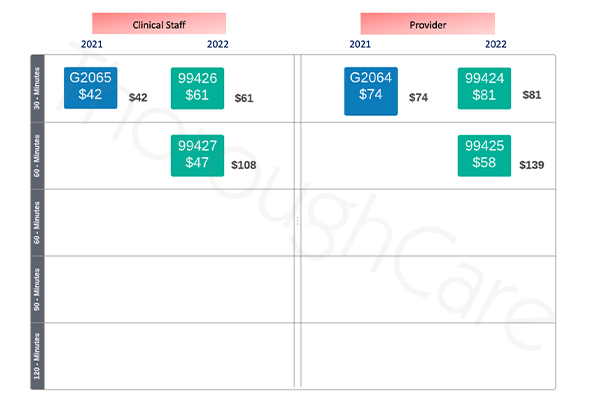 For a patient with one qualifying chronic condition, but not two conditions, PCM can be an appropriate program. That said, if your patient does require attention for at least two high-risk conditions, CCM will be a more fitting, as well as more profitable, option.
For a patient with one qualifying chronic condition, but not two conditions, PCM can be an appropriate program. That said, if your patient does require attention for at least two high-risk conditions, CCM will be a more fitting, as well as more profitable, option.
Higher Care Management Reimbursement for RHCs and FQHCs
Rural and federally qualified clinics may now utilize CPT code G0511 for a higher billing rate.
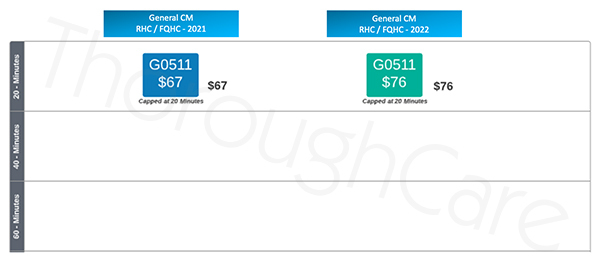 The code applies to “general care management,” but its broad scope can allow for CCM and BHI, as well as RPM. This increase showcases CMS’s interest in expanding access to such programs for patients living in rural areas, where immediate access to healthcare may not be available.
The code applies to “general care management,” but its broad scope can allow for CCM and BHI, as well as RPM. This increase showcases CMS’s interest in expanding access to such programs for patients living in rural areas, where immediate access to healthcare may not be available.
A Slight Rate Decrease for Remote Patient Monitoring
Though the program is popular, CMS has cut the rate for RPM and its related reimbursements.
The following chart details the new changes versus what was established in 2021.
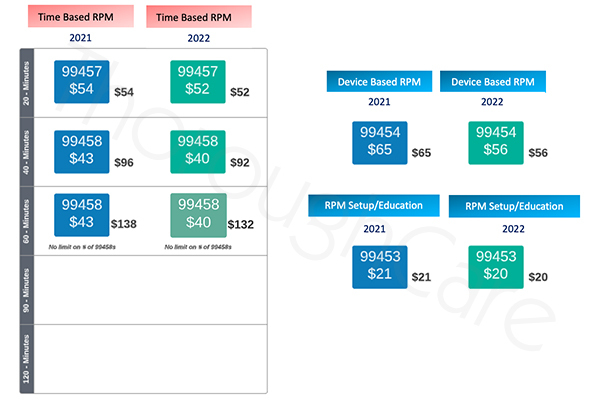
As you can see, the cuts are across the board, from billable time to device use — though small.
To offset this loss, it may make sense to promote CCM enrollment with your RPM patients. This way, you can instead bill for 20 minutes of CCM time, receiving a higher rate.
At approximately $62 for 20 minutes of non-complex CCM service, it’s still possible to pair this CPT code with RPM device use. This strategy would net about the same as 2021’s total RPM reimbursement (billable time + device use).
CMS Introduces Remote Therapeutic Monitoring
There’s a bit of buzz about this new program, though its application may, so far, be limited.
CMS has aligned Remote Therapeutic Monitoring (RTM) to conditions of the musculoskeletal and respiratory systems. The program is intended to be non-physiological in nature. Its attention resides with therapy, adherence, and response.
RTM will work similarly to RPM, in that patients will be equipped with specific devices and use them at home to monitor their conditions. RTM’s billing structure also mirrors RPM’s.
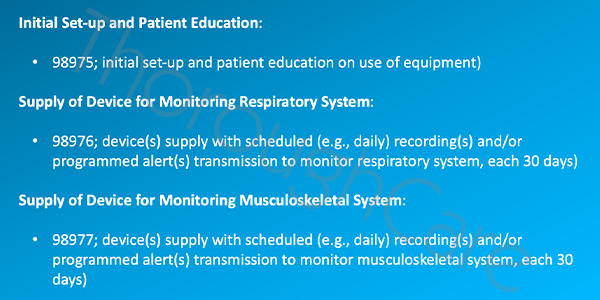
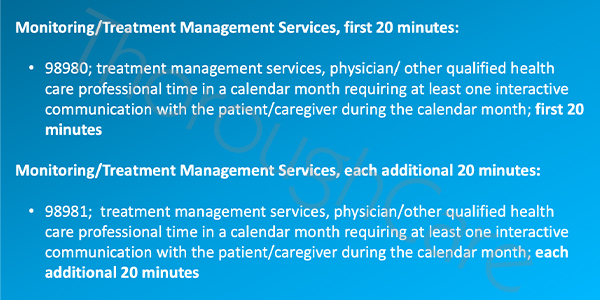
Its five CPT codes are different, yet the rates are the same as RPM. They are detailed below.
It is important to note a key difference between RTM and RPM. Clinical staff cannot provide RTM services unless they are directly supervised by a physician or other qualified professional.
The program is also only billable for physical therapists, occupational therapists, dietitians, clinical psychologists, and other QHCPs.
In the future, we hope CMS may soften these rules, as well as expand RTM’s application to other conditions.
Concurrent Billing for CCM and Transitional Care Management By RHCs and FQHCs
General care providers have already been able to do this, but rural and federally qualified clinics may now bill for both CCM and TCM in the same month.
Such clinics can utilize CPT code G0511 for 20 minutes of CCM service.
CPT Codes 99495 and 99496 will account for TCM reimbursements. Each is applicable based on the complexity of medical decision-making required for TCM services.
Both programs tend to pair well together, as TCM covers immediate care after a hospital discharge, and CCM provides long-term care for two or more high-risk conditions.
Both reduce readmissions.
Care Coordination Software for Medicare’s Wellness Programs
Without the right resources or strategy, Medicare’s wellness and preventive programs can be hard to manage. Specific rules and regulations can run amiss. Workflows will lack efficiency.
Care coordination software can be a good solution to these potential problems.
ThoroughCare offers a software solution equipped to streamline these programs. It can guide your staff through processes, record billable time, and collect and analyze patient data.
For any client, we offer extensive training opportunities and learning resources. Our tech support team is readily available, and we integrate with several of the leading EHR providers.
Our software modules are designed exactly to federal rules and regulations for Medicare’s preventive, value-based care programs, and they’re easy to use and understand.
Our software is designed by clinicians for clinicians. Take a look for yourself.
Watch a free software demonstration, and see exactly how care coordination software can benefit your practice and your patients.


.jpg)
