Behavioral Health | Behavioral Health Integration
BHI Adoption and Reimbursement Support Primary Care Integration
Medicare beneficiary statistics demonstrate the need for some level of behavioral health integration with primary care:
- 25% of Medicare beneficiaries experience mental illness
- 40% experience mental illness or a substance use disorder
- 23% of patients with serious mental illness (SMI) are covered by Medicare
- 4.2% of total Medicare spending went to mental health services
- 8.5% went to additional medical spending associated with mental illness
One study found that having a mental health disorder was associated with substantially higher spending on other medical conditions, increasing total Medicare spending related to mental health disorders three-fold.
Behavioral Health Integration helps primary care treat two types of patient issues
While primary care is already stretched to its limits, behavioral health integration through primary care is an important initiative increasingly supported through reimbursement, special programs, and technology.
Here’s why: 75% of primary care practices engage in some level of behavioral health in their appointments, and two-thirds of PCPs can’t connect patients with accessible follow-up services.
But, there’s a deeper motivation for primary care to integrate physical and behavioral health.
Primary care physicians are seeing two types of patients:
- The patient with chronic conditions that are creating stress-induced symptoms and behavioral health issues like depression and anxiety disorders
- The patient with an existing mental health condition who is at high risk for, or already experiencing, one or more chronic conditions like diabetes, obesity, and high blood pressure
Both of these scenarios increase the likelihood that patients will be unable to self-manage both physical and mental conditions. Or, they’ll be unable to adhere to care plans and medication regimes adequately.
A Medicare program called Behavioral Health Integration (BHI) is considered an effective strategy for improving outcomes for millions of Americans with mental or behavioral health conditions.
BHI trends show increased adoption
BHI has been shown to improve outcomes for individuals with behavioral health conditions, reduce healthcare costs, and improve access to care.
According to America’s Health Insurance Plans (AHIP), recent research shows that the adoption of behavioral health integration is growing. Their report highlighted three trends:
- Commercial health plans saw an increase in two BHI codes between 2018 and 2021
- Payment from commercial plans for BHI codes increased 18% from 2018 to 2021
- Payment for the BHI codes has been higher in the commercial market than Medicare plans
Figure 1 from AHIP’s report shows the significant increase in commercial billing for four BHI codes under the Collaborative Care Model (CoCM) and General BHI programs (BHI). Figure 2 highlights how payors have evolved their strategies since 2017, relying more heavily on BHI care managers, readmission prevention programs, and CoCM.
AHIP summarized that this trending increase in adoption is likely due to four factors:
- Greater awareness of the existence of the BHI billing codes
- Greater awareness of the evidence for the value of BHI
- More primary care physicians are willing to take on mental and behavioral health
- Legislative efforts to promote integrated behavioral health
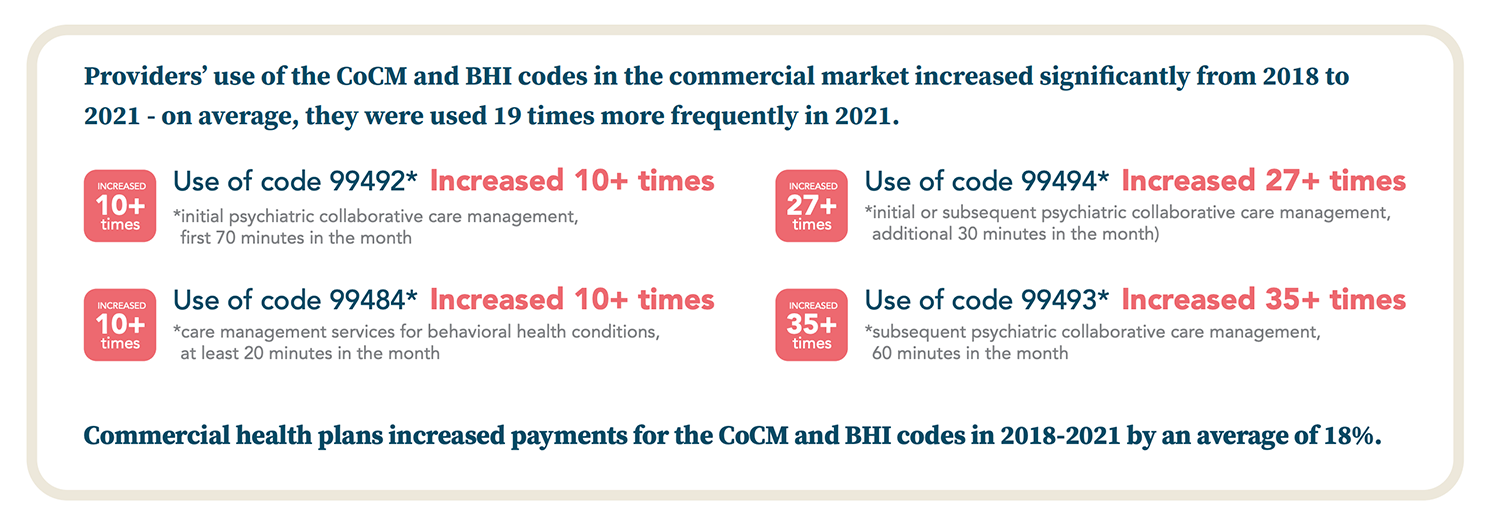
Figure 1: Commercial health plans have seen a significant increase in BHI-related billing codes. Source: PsychU
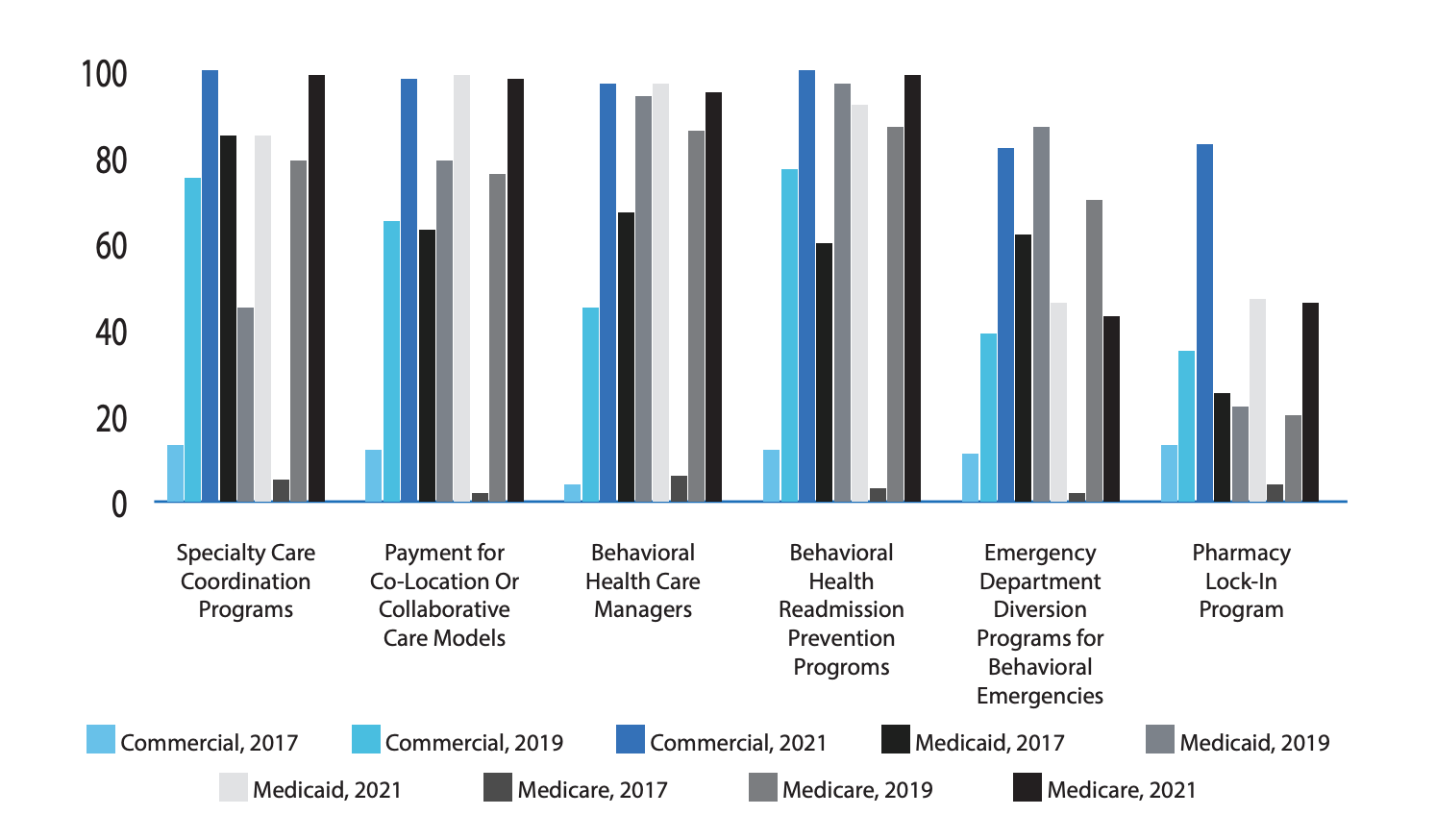
Figure 2: Various coordination of care strategies deployed by various health plans. Source: PsychU
Available and expanding BHI programs support primary care adoption
Medicare and Medicaid have developed payment models to support BHI, including both the Behavioral Health Integration Program and the Collaborative Care Model. These models offer financial incentives for primary care providers to integrate behavioral health with existing services.
General BHI is a monthly service that ThoroughCare supports. It includes “core” service elements required for reimbursement, such as:
- Evidence-based and systematic assessment and monitoring
- Care plan creation and oversight
- Care plan revision for patients whose conditions are not improving adequately
- Ongoing touchpoints with a designated care team member
Unlike the Psychiatric Collaborative Care Model, the General BHI model does not require a psychiatric consultant or a designated behavioral health care manager. This makes it more accessible to primary care practices.
General BHI practitioners use CPT code 99484 to bill monthly services, such as:
- Initial assessment
- Initiating visit (if required, separately billed)
- Administration of applicable validated rating scale(s)
- Systematic assessment and monitoring using applicable validated clinical rating scales
- Care planning by the primary care team jointly with the beneficiary, with care plan revision for patients whose condition(s) are not improving
- Facilitation and coordination of behavioral health treatment
- Continuous relationship with a designated member of the care team
Figure 3, from the American Academy of Family Physicians (AAFP), outlines the main differences between CoCM and General BHI, highlighting how primary care can have a lower barrier to entry with this program.
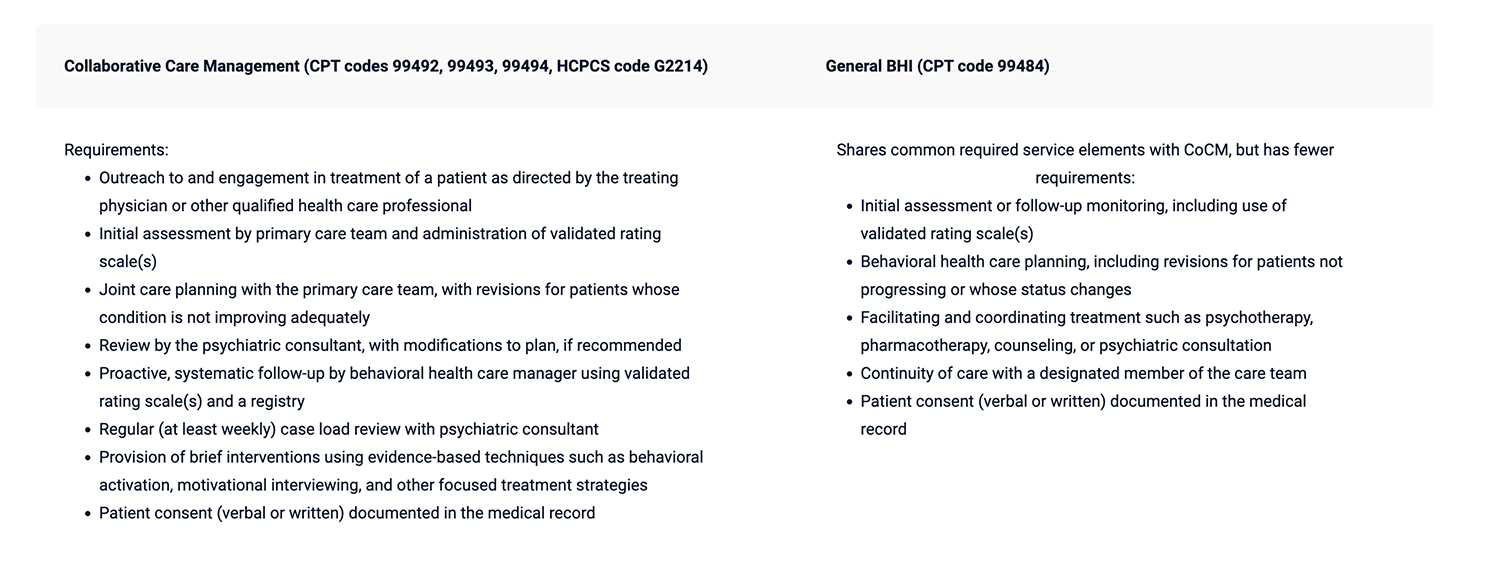
Figure 3: Side-by-side comparison of coding requirements for CoCM vs. general BHI services. Source: AAFP
New CMS program supports BHI innovation
Mental health care is in high demand. Psychologists are leveraging tech and peers to meet the need.
The Centers for Medicare & Medicaid Services (CMS) is launching a new program in 2024 to test approaches to addressing beneficiaries’ behavioral and physical health issues and health-related social needs.
Called the Innovation in Behavioral Health (IBH) model, participants in eight states will be equipped with the necessary resources to facilitate integrated care, including infrastructure payments to support health IT capacity building, electronic health records, and more.
What’s unique about this program is that it focuses on reversed integration—bringing physical health services into behavioral health programs through interprofessional care teams. These teams will consist of behavioral and physical health providers and community-based support.
The model will incentivize practice participants to collaborate on screening, assessing, and coordinating a patient’s physical and behavioral health needs.
According to CMS, “a person-centered approach to addressing whole-person health represents a ‘no wrong door’ approach that prioritizes close collaboration with primary care and other physical health providers to support all aspects of a patient’s care.”
Primary care can manage chronic conditions with BHI
Primary care practices that already offer Chronic Care Management can co-enroll patients in Behavioral Health Integration to maximize the strengths of both programs.
This is an effective combination for either type of patient – those with chronic conditions who are struggling with behavioral health, or those with a mental health condition who are beginning to experience chronic health conditions.
Tapping into both programs offers four benefits:
Physical and mental health issues receive due attention individually but can be managed through ThoroughCare under one patient profile. This provides robust information across both areas, giving clinicians and the broader care team insight into potential gaps and exacerbations.
The broader care team can share roles between physical and mental healthcare. Physicians can elicit the help of a care manager or nurse practitioner with mental health experience or training to support various aspects of treatment. They can then focus more on medication, diagnosis, and chronic condition management.
Combining CCM with BHI can enhance patient care plan adherence. Many patients who experience behavioral health issues struggle with self-management and medication or lifestyle compliance. CCM and BHI provide a powerful combination of continual support and oversight.
Adding BHI makes primary care more attractive and competitive for value-based contracting and partnerships. Providing integrated services through care management demonstrates the ability to support high-quality, cost-effective care.
ThoroughCare enables seamless care management across behavioral and physical programs
Recent adoption trends in behavioral health integration and new payment models offer an opportunity for primary care to engage Medicare beneficiaries in combined physical-mental treatment.
ThoroughCare provides a complete, end-to-end platform that equips care teams to manage one or more care management programs for individual patients.
Through our workflow for Behavioral Health Integration, we simplify the process so providers can focus on engaging patients. ThoroughCare:
- Streamlines the creation of patient care plans
- Supports staff workflows with guided assessments
- Helps motivate patients through clinical recommendations
- Analyzes patient risk factors and generates clinical recommendations
- Tracks and logs BHI services for an audit-proof record of care
- Supports validated assessments to identify behavioral health conditions, including PHQ-9 (Depression), GAD-7 (Anxiety), CAGE (Alcohol), DAST-10 (Substance Abuse), and MDQ (Mood Disorders)



